If you’ve ever wondered where confidence, competence, and a bit of clinical magic are made, look no further than the Ibn Sina Simulation Lab — the beating heart of hands-on learning at Thunder Bay Regional Health Sciences Centre (TBRHSC). This immersive, high-energy space is where students and clinicians step into realistic scenarios and sharpen their skills in ways that truly bring health care education to life.

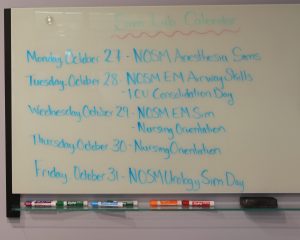
Photo 1: Leanne Baird, Manager of the Ibn Sina Simulation Lab (Sim Lab) invited us in for a closer look at this dynamic space. Her passion for experiential learning and patient-centred training was contagious from the moment she welcomed us in. When asked what she likes about her job, she exclaims “Everything! My job is the best. Let me show you why!”
Photo 2: Baird starts by explaining that the Sim Lab is a learning hub for students, clinicians, and allied health care teams. Continuing professional development takes on a new level of excitement when professionals can refresh skills, trial new procedures, or participate in high-energy scenario training. In a field that evolves daily, simulation ensures health care providers stay sharp, confident, and ready for anything. “The Sim Lab is hopping,” smiles Baird. “The schedule changes every week. We are a teaching Hospital, so we have every type of health care learner.” The photo shows an example of a training schedule for the week.



Photos 3, 4, 5: “It’s a high-impact, no risk environment,” shares Baird. “Imagine walking into a room that looks and feels exactly like a real hospital room with monitors beeping, equipment ready, and a patient [a high-fidelity mannequin] that can talk, breathe, bleed, and even give birth. We can set the space up like an operating room, a birthing suite, whatever is necessary for the specific medical skill the instructor is teaching.” This is where learners get to try, fail, try again, and ultimately master essential skills without ever putting a real patient at risk. “It’s hands-on learning at its most dynamic and empowering.”


Photos 6 and 7: From the control room, Leanne controls various aspects of the high-fidelity mannequin, including pupil dilation, chest movement and voice. She demonstrates by speaking through the microphone and the mannequin suddenly comes to life, blinking and talking. The blend of realism, innovation and teamwork, creates a dynamic and exciting learning environment.



Photos 8, 9, 10: Some clinical events happen only a few times in a clinician’s entire career, but when they do, there is no margin for error. The Sim Lab allow teams to rehearse skills that are High Acuity, Low Occurrence (HALO) until they can respond with calm precision. It is all about building muscle memory, confidence, and clinical excellence that directly translates into safer patient care.

Photo 11: After every scenario, teams come together for structured debriefing, providing a safe, supportive space to reflect, share insights, and refine performance. These conversations are where breakthroughs happen. Learners unpack what went well, what could be improved, and how to elevate their practice. It’s the heartbeat of a culture focused on continuous growth and excellence.
When it comes to a project as large as the Cardiovascular Surgery Program, it truly takes a village—from the construction, safety, and communication teams, to those responsible for operational readiness and clinical integration, to other partners including the provincial government and donors to the Thunder Bay Regional Health Sciences Foundation, providing essential financial support. Below is a closer look at some of the dedicated team members and partners currently bringing the capital portion of this project to life.
TBRHSC Cardiovascular Surgery Program Construction Project Management Team
Northwestern Ontario has the highest rates of cardiovascular disease in the province. Patients often have to travel long distances for specialized cardiac care, which can create logistical, financial, emotional and health challenges. To address this, Thunder Bay Regional Health Sciences Centre (TBRHSC) prioritized bringing cardiovascular care closer to home for the people of Northwestern Ontario through a collaborative “Two Sites, One Program” model with University Health Network’s Peter Munk Cardiac Centre.
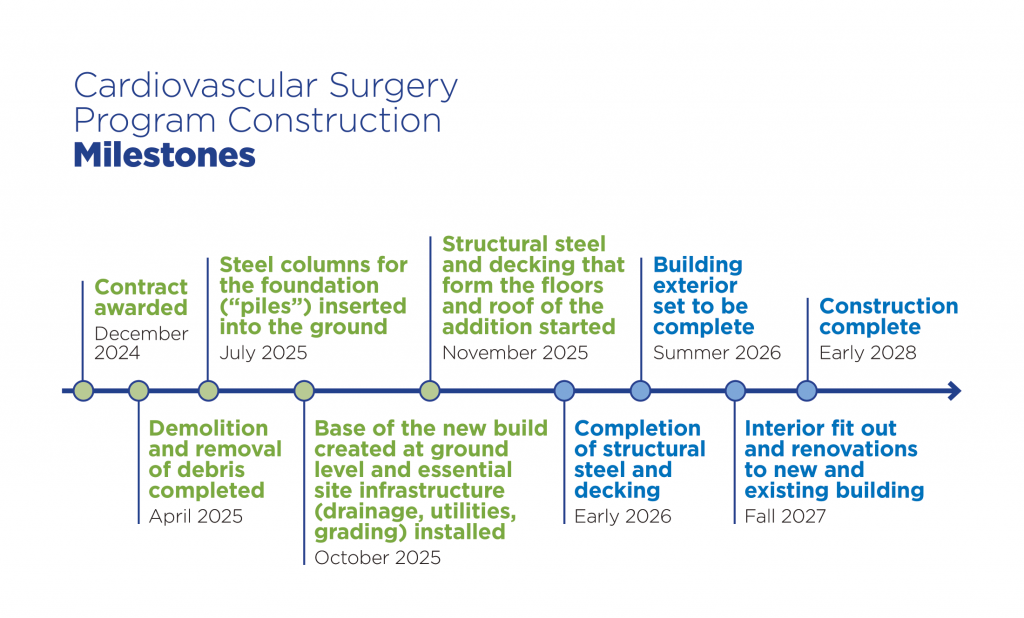
Starting in 2013, the organizations collaborated on a comprehensive plan aimed at enhancing patient care and advancing regional clinical outcomes in cardiovascular health. The first phase of the plan focused on the development and implementation of the vascular surgery program; the second phase consisted of developing a comprehensive Cardiovascular Surgery Program, expanding services significantly. And with the expanded services comes the requirement for more space, which requires a multi-stage approval process set out by the provincial government.
By 2015, internal planning was well underway, and the pre-capital submission was sent to the Ministry of Health. Over the next several years, the project moved through several important planning stages—including the Functional Program, Detailed Planning and Design, and development of Construction Documents.
Then in June 2024, the project reached a major milestone: approval from the Ministry of Health to tender construction. A construction contract was awarded in December 2024, officially kicking off the next phase of bringing cardiovascular surgery closer to home.
And what started more than a decade ago as an exciting clinical vision for TBRHSC is now becoming a reality, with construction well underway on 76,000 square feet of new and renovated clinical and support spaces for the new Cardiovascular Surgery Program.
Behind the bricks and mortar of this project is a dedicated group of professionals working together to bring the expansion to life. The Construction Project Management team involves a wide range of expertise, from clinical safety and communications to design, procurement, and finance—all working in harmony to ensure the project meets the highest standards.
It truly takes a village to bring a project of this scale to life—from coordinating construction to ensuring safety, communication, operational readiness, and clinical integration. Here’s a look at the dedicated team members and partners driving the capital project forward:
TBRHSC Cardiovascular Surgery Program Construction Project Management Team
- Ryan Sears, Project Director: Provides overall leadership and oversight, including managing time, budget, quality, internal coordination, risk, and communication.
- Aaron Bruno, Project Planner: Leads construction review, consultant coordination, project planning, and scheduling. Oversees change orders, quality assurance, financial reviews, and communication.
- Daniel Sedano, Project Coordinator: Keeps a close eye on daily construction activities, ensuring quality and spec compliance. Coordinates departments, schedules, and consultant inputs.
- Clayton MacDonald, Occupational Health and Safety (OH&S): Reviews safety plans and ensures the site meets health and safety standards.
- Stephanie Erickson, Infection Prevention and Control (IPAC): Ensures infection control protocols are integrated into every stage of the construction process.
- Raiili Pellizzari, Communications and Engagement: Leads all project-related communications—keeping internal teams and the community informed and engaged.
- Darin Pretto, Maintenance: Coordinates construction activities within the existing facility, including system shutdowns and tie-ins.
- William White, Procurement: Leads procurement of all hospital Furniture, Fixtures, and Equipment (FF&E) for the expansion.
- Ted Wyant, Finance: Oversees TBRHSC financial planning and coordination with the Thunder Bay Regional Health Sciences Foundation and Ministry of Health.
External Partners and Consultants
- BTY Consulting Group: Supports with project administration, construction reviews, consultant coordination, and FF&E management.
- FORM Architecture, Parkin Architects, HH Angus and Associates: Manages the construction contract, issues formal documents (like change orders), responds to contractor questions, and certifies progress payments.
- CES Engineering: Acts as the Commissioning Agent—ensuring building systems (like HVAC and electrical) are installed and functioning exactly as designed.
- Tom Jones Corporation: The General Contractor, managing construction and sub-trades, oversees the entirety of the construction project and brings the detailed construction documents to life.
As construction progresses, this collaborative team remains committed to creating a facility that reflects the high standard of care TBRHSC is known for. When completed, the new cardiovascular space will not only enhance local care options but also reduce the need for patients to travel for specialized treatment.
“This project has always been about delivering better care, closer to home,” said Ryan Sears, Project Director. “Patients and families in our region face the emotional and physical burden of traveling over 1,300 kilometers by air to receive cardiac care. That’s not just a journey—it’s a separation from their family or support networks and sometimes, even a barrier to treatment.”
“Care closer to home means more than convenience in a difficult time. It means safety and the peace of mind that comes from knowing expert care is just down the road. It means families can stay together during some of the most challenging moments of their lives. To me, this project is not just steel and concrete. It is a promise that the people of our community matter, their health matters, and that they shouldn’t have to leave home to get the care they deserve,” concludes Sears.

(L-R) TBRHSC Cardiovascular Surgery Program Construction Project Management Team: William White, Procurement Specialist; Daniel Sedano, Project Coordinator; Aaron Bruno Project Planner; Clayton MacDonald, Safety Consultant; Darin Pretto, Maintenance and Energy Lead; Stephanie Erickson, Manager, Infection Prevention and Control; and Raiili Pellizzari, Communications Specialist and Project Lead. Not pictured: Ryan Sears, Director, Capital and Facility Services; and Ted Wyant, Manager, Accounting and Management Reporting.

TBRHSC Cardiovascular Surgery Program construction project management, consultants, and contractor.
As we conclude 2025, I am proud to reflect on a year marked by resilience, innovation, and unwavering commitment to our mission of delivering exceptional care to every patient, every time. Over the last year, Thunder Bay Regional Health Sciences Centre (TBRHSC) has continued to advance clinical excellence, strengthen operational performance, and invest in our people and infrastructure. The achievements stand as a testament to the dedication of our staff, the leadership of our senior team, and the steadfast support of our Board of Directors. Together, we have not only met the demands of today but have also laid a strong foundation for the future of compassionate, patient-centered care.
We are proud to welcome five new physicians this last quarter: Drs. Barbara Gunka (Hematologist), Elham Talachian (Paediatrician), Mohamed Elkoushy (Urologist), Siavosh Nasseri-Moghadda (Gastroenterologist) and Rasoul Javan (Cardiologist). These highly skilled physicians have joined our team of professionals committed to innovation, collaboration, and the highest standards of clinical practice. Their expertise, compassion, and dedication to excellence will complement our existing professional staff and continue to advance our mission to provide patient-centered care to the people of Northwestern Ontario. Please join us in welcoming them to our community.
Other exciting news from this past month includes the announcement of $22,815,488 in grants from the Thunder Bay Regional Health Sciences Foundation. The funds will be used to purchase essential equipment at TBRHSC and regional hospitals. This represents the largest single commitment the Foundation has ever made — made possible through the remarkable generosity of donors, event participants, and Thunder Bay 50/50 supporters. Thank you to our donors for their incredible generosity, and to the Health Sciences Foundation for their dedication to enhancing care in our region.
This month, we celebrate International Volunteer Day (December 5). Volunteers are an essential part of our Hospital community, generously sharing their time and talents to enhance the lives of our patients, families, and staff. I would like to take this opportunity to recognize and extend a heartfelt thank you to all our dedicated volunteers for their invaluable contributions.
To further enhance care, one of the key goals within our Strategic Plan 2026 is to build a Sustainable Future to ensure our health future. As part of this commitment, we aim to inspire the next generation to pursue careers in health care.
Recently, TBRHSC hosted two exciting events: Take Our Kids to Work Day and the Indigenous Career Experience that introduced local students to the wide range of possibilities available in health care. Take Our Kids to Work Day is an annual experiential learning opportunity for Grade 9 students across Ontario. During their visit, students toured various Hospital departments, gaining insight into different health care professions and volunteer opportunities. Similarly, during the Indigenous Career Experience, students explored diverse roles within TBRHSC and participated in hands-on activities designed to spark curiosity and connection to the health care field.
Through these initiatives, we hope to ignite a passion for helping others and encourage students to envision themselves as future health care professionals — contributing to a sustainable future and ensuring the health of generations to come.
As we move into 2026, I extend my sincere appreciation to our staff, professional staff, learners and volunteers for their continued dedication and professionalism. Together, we will build on this year’s progress and remain focused on delivering the highest quality of health care to the people of Northwestern Ontario. On behalf of the Board, I wish everyone continued success in the year ahead.
As we approach the 2025/26 respiratory season, Thunder Bay Regional Health Sciences Centre is taking steps to help protect patients, families, and health care teams from respiratory and influenza-type illnesses.
Starting December 4, 2025, all staff, professional staff, learners, volunteers, and Essential Care Partners/Care Partners will be required to wear a Level 3 procedure mask when in the Emergency Department, on specific units, and when entering any inpatient room.
Here’s what you need to know:
1A Inpatient Units (1A Medicine and 1A Acute Oncology)
- A Level 3 mask is required at all times while on the unit, including inside patient rooms and anywhere in the clinical area.
All Other Inpatient Units
- Staff, professional staff, learners and volunteers must wear a Level 3 mask when: entering a patient room, providing direct patient care, transporting patients, or when unable to maintain six feet of physical distance.
- ECPs/CPs must wear a Level 3 mask when entering a patient room or when unable to maintain distancing.
Emergency Department
- Staff, professional staff, learners and volunteers must wear a Level 3 mask when entering patient rooms, providing care, transporting patients, or when distancing isn’t possible.
- Patients and ECPs/CPs must wear a Level 3 mask at all times in the Emergency Department.
Masks are available at all public entrances on our sanitizing stands, and hand sanitizer dispensers are located throughout the Hospital. We strongly encourage everyone to practice hand hygiene and to wear a mask to help reduce the spread of illness.
Our Infection Prevention and Control team continues to monitor infection trends closely. Any updates to masking requirements or other safety measures will be communicated clearly and promptly.
Thank you for your continued cooperation in helping us keep our Hospital and community safe.
Renovations are underway in the Emergency Department triage area at Thunder Bay Regional Health Sciences Centre (TBRHSC). This project will transform the reception, registration and triage areas to better serve our community, and enhance patient and staff flow.
Construction started this week, and while you may notice some changes around the Emergency Department, public access will remain open through the current entrance. Check in, registration, and triage will also remain in place and signage will be posted to aid in navigating the area. Your safety is our priority, so please follow all signage and respect construction areas.
What to expect when arriving at the Emergency Department entrance:
- Temporary walls around the construction area to ensure safety and security.
- Temporary changes to hallways and the waiting area.
- There may be slight changes to how you’re routed through reception, registration and triage.
Signs will be posted to aid in navigating these changes.
Stay tuned for more updates, and thank you for your continued support as we work to improve the patient experience at TBRHSC.
Over 60 students from school boards across Thunder Bay were on-site at Thunder Bay Regional Health Sciences Centre (TBRHSC) on November 19 to explore many different health care career and volunteer options.
In its fifth year, the Indigenous Career Experience is dedicated to inspiring Indigenous youth by providing essential insights into diverse health care career opportunities and by building relationships with TBRHSC. A significant aspect of the program is connecting with high school students before they make final decisions about post-secondary education. Through hands-on learning experiences, it ignites their enthusiasm for pursuing a future in health care. Additionally, the initiative supports the recruitment of Indigenous professionals within the health care sector.
A special part of this year’s event was the naming of the program with a traditional Spirit Name. Elder Aaron Therriault gifted the name ‘Kinomagai Akosii-agamong Anokiiwin’, which translates to ‘teaching hospital, career or work’. The name represents the work that our Hospital does, as it is a place for teaching and learning.
Students experienced a day filled with tours, presentations, and hands-on activities designed to provide them with an authentic feel of various health care roles. Students had the opportunity to interact with managers and staff, ask questions, and learn about the educational pathways required for various positions.
“It was a fun day. I think the hands-on activities were the best part. Using surgical tools in the operating room was super cool. I also really enjoyed learning about Indigenous traditions like drumming and smudging, which I don’t get to do often,” said a grade 10 student from Hammarskjold High School. “The ‘Amazing Race’ activity was really fun and interactive. I appreciated how the staff explained everything and answered our questions.”
The departments that participated — the Operating Room, Medical Device Reprocessing Department, Nutrition and Food Services, Maintenance, Miskwaa Biidaaban, Interprofessional Education, and Volunteer Services — played a vital role in making this day a valuable and fun learning experience for the students.
“It was such a pleasure to run our Amazing Race Workshop with students from all grades and schools across Thunder Bay,” said Holly Freill, Interprofessional Educator. “Everyone jumped in with enthusiasm, making it a fun day filled with challenge, teamwork, and lots of laughter,” added Jennifer Gadioma, Interprofessional Educator.
Take Our Kids To Work Day (TOKTWD) — which took place on November 5 — is an annual experiential learning opportunity for Grade 9 students across Ontario.
Thunder Bay Regional Health Sciences Centre hosted over 40 grade 9 students from schools across the city. A team member from Human Resources provided a guided tour through the Hospital to seven departments including the Ibn Sina Simulation Lab, Medical Device and Reprocessing Department (MDRD), Operating Room, Biomedical Engineering/Maintenance, Pharmacy, Diagnostic Imaging, and Nutrition and Food Services.
Additionally, students received a presentation from Volunteer Services to learn more about volunteer opportunities and from Infection Prevention and Control regarding the importance of hand hygiene.
By participating in TOKTWD, students are able to learn about the variety of careers within the Hospital and in health care. This day also creates a great opportunity for employee engagement within the workplace. This event encourages team building, productivity, social interactions and employee involvement.
Thank you to everyone who made this year’s edition of TOKTWD a success!
Originally published in Health System News
Stroke care in Northwestern Ontario faces unique challenges, including vast geographic distances, limited stroke specialist access, and variable transport infrastructure. Addressing these barriers demands breakthrough innovations that harness technology and data to improve patient outcomes and system efficiency.
The Northwestern Ontario (NWO) Navigate Stroke application is a cutting-edge technological innovation developed to assist health care providers in Northwestern Ontario with efficient navigation of stroke patients to the most appropriate levels of care. This interactive digital tool integrates geomapping technology and machine learning algorithms to provide real-time decision support in navigating patients through the complex, geographically dispersed stroke care network of Northwestern Ontario.
“This app is tailored specifically to the unique challenges of our region,” said Dr. Ayman Hassan, Neurologist at Thunder Bay Regional Health Science Centre (TBRHSC) and one of the co-developers of the app. “By using continuous and varied data inputs, health care providers are able to make informed decisions for their patients that can lead to better patient outcomes, better care coordination, and enhanced system efficiency.”
The application consolidates critical information including patient location, stroke-specific timelines such as the last known well time, availability of diagnostic imaging at different health care facilities, and estimated travel times based on historical and current data. By combining these data points, the app offers health care providers the fastest routing options and the most appropriate access to stroke treatment sites, helping to reduce delays and improve patient outcomes for stroke patients across Northwestern Ontario. The system leverages machine learning decision models to accurately predict transport time intervals and coordinate stroke management pathways, ensuring alignment with evidence-based stroke care protocols.
This app was designed through a collaborative effort involving data scientists, clinicians, and emergency medical services operating within Northwestern Ontario: Thunder Bay Regional Health Sciences Centre, Northwestern Ontario Regional Stroke Network, Thunder Bay Regional Health Research Institute, Lakehead University (Computer Engineering department) and Ornge, with funding through Northern Ontario Academic Medicine Association (NOAMA).
The NWO Navigate Stroke app exemplifies how artificial intelligence and data-driven innovations are transforming health care delivery, especially in rural and remote settings.
The app is freely available on Android, iOS, and web platforms, empowering clinicians working both locally and remotely to make timely, informed decisions regarding acute stroke care. This innovation not only advances patient care but also represents a significant step forward in using AI and data insights to address the logistical and clinical challenges of stroke systems in complex health care environments.
The NWO Navigate Stroke app showcases the value of regional collaboration in developing AI-based tools, the importance of customizing technological solutions to local contexts, and the critical role of data integration for real-time clinical decision-making. It is a beacon of innovation offering insight into how AI-driven navigation systems can shape the future of stroke care in Ontario and beyond.
Teamwork, dedication, and excellence were on full display during Thunder Bay Regional Health Science Centre (TBRHSC)’s recent Minimum Staffing Drill. This annual exercise, mandated by the Ontario Fire Code, is coordinated by TBRHSC’s Emergency Preparedness and Interprofessional Education teams, and in partnership with Thunder Bay Fire Rescue (TBFR).
The Hospital-wide drill tests the ability to safely evacuate an in-patient unit during hours with minimum staffing levels. Every year the drill focuses on a different area of the Hospital to enhance these capabilities.
During the drill, more than 40 volunteers acting as mock patients and family members were evacuated from 3B (Surgical Inpatient) to 3C. This enhanced the exercise by providing the opportunity for staff to practice communication techniques and apply patient and family centred principles.
Volunteer Barb Rickards was happy to join in the learning opportunity for staff. “I had so much fun being a mock patient family member,” she exclaimed. “It was interesting to see what happens behind the scenes during a Hospital drill and how everyone stays calm and focused. The drill gave me a real appreciation for how much coordination and teamwork goes into providing safe patient care. It was great to see how the team worked together under pressure.”
The “room of origin” (where the mock fire started) was evacuated within 36 seconds and the entire unit was evacuated in 16 minutes and 44 seconds. Teams demonstrated strong communication and problem-solving skills while maintaining patient care standards. The exercise also provided valuable insight into workflow efficiency, communication processes, and cross-departmental support. Additionally, TBFR was impressed with how clean Anne Purves, Manager 3B, and her staff kept the unit, with tidy sprinkler heads and properly stored equipment.
“This was the first year we’ve had evacuation door tag markers in place, which will help accelerate the process for searching rooms and identifying them as evacuated,” said Mēsha Richard, Emergency Preparedness Lead. “Staff did an amazing job utilizing the new tool, but more familiarity will be beneficial. Everyone needs to trust that if a door is marked it means that space was already searched and cleared.”
“Overall, this drill gave us a realistic picture of how we can continue to deliver excellent care even under challenging circumstances,” added Richard.
The drill concluded successfully, with lessons learned documented and action plans developed to enhance exercise realism and improve future response strategies. Key takeaways included the importance of clear communication and delegation, as well as wayfinding to ensure responders follow the safest routes in and out of the impacted unit.
Every day, patients, families, and health care teams at Thunder Bay Regional Health Sciences Centre (TBRHSC) face choices that do not always have an easy answer. Whether it is deciding on a treatment plan or navigating differing opinions about what’s best for a loved one, these moments can be emotional and complex. That is where the Hospital’s ethics service can help.
Ethics is about doing what’s right — not just medically, but in a way that respects people’s values, beliefs, and experiences. The ethics service at TBRHSC supports patients, families, and staff in exploring difficult questions with compassion and clarity. “The ethics service helped us find a path forward that balanced safety with what mattered most to the patient,” shared one care team member. “It helped everyone feel heard.”
Consider this example: a patient nearing the end of life was torn between wanting to spend as much time as possible at home with family and accepting a treatment that might extend life but require a long hospital stay. The care team, along with the Bioethicist, helped the patient and family talk openly about what mattered most — comfort, time together, and dignity. Together, they reached a decision that aligned with the patient’s values and wishes.
This is ethics in everyday care — helping people make informed, values-based decisions that reflect what’s truly important to them.
At TBRHSC, ethics is woven into exceptional care every day. The Bioethicist and Ethics Committee, made up of staff and Patient Family Advisors, offer guidance and support for a wide range of situations — from bedside decisions to Hospital-wide policies.
During National Ethics Week (November 2–8), TBRHSC joins hospitals across Canada in recognizing the vital role of ethics in compassionate, patient-centered care — care that honours people’s values, builds trust, and supports the well-being of the whole person.
On October 8th, Thunder Bay Regional Health Sciences Centre (TBRHSC) opened its doors and welcomed over 300 attendees — from high school students to those looking for a new career path — to explore the world of health care careers at the Open Doors Career Showcase.
Taking place in the Hospital’s cafeteria, the experience allowed attendees to understand the wide range of roles available in the health care sector. Individuals discovered career options they may never have considered previously. Whether their interests were in clinical, technical, or administrative fields, everyone saw there is a place for them in health care.
“Experiencing the health care environment firsthand helps people truly understand the wide range of roles available,” says Jeannine Verdenik, Vice President, People and Culture at TBRHSC. “This event opens doors — literally and figuratively — for individuals to discover career options.”
Over 30 departments participated, with representatives at each booth ready to answer questions and share insights about the qualifications needed for various positions. Guided tours of Hospital departments highlighted diverse career paths in many roles. Participants visited Diagnostic Imaging, Rehabilitation Services, and Medical Device Reprocessing and engaged in clinical simulations in the Simulation Lab.
“The event was incredibly well attended and very well organized,” said Leanne Baird, Simulation Program Manager, who hosted a tour at the Showcase. “It was such a valuable opportunity to highlight the many diverse career opportunities available at TBRHSC.”
The feedback from attendees was overwhelmingly positive. TBRHSC plans to host this event annually, allowing more individuals to explore career options in the health care sector. Stay tuned for more information about next year’s Showcase.
For those who could not attend but are interested in a health care career or are curious about why TBRHSC is a great place to work, grow, and thrive, the Human Resources team is available for inquiries via email at TBRHSC.HumanResources@tbh.net or by calling (807) 684-6227.
Breast cancer is the most common cancer among women in Ontario, yet almost 50% of those who are eligible for breast screening in Northwestern Ontario don’t get checked regularly. For some, it’s the fear of the unknown. For others, it’s not knowing when to start, how often to go, or whether their personal circumstances affect their eligibility.
To makes things easier, here are answers to some of the most common questions about breast cancer screening.
Who is eligible for breast screening in Ontario?
The Ontario Breast Screening Program (OBSP) recommends that most eligible women, Two-Spirit, trans, and non-binary people ages 40 to 74 get a mammogram every two years.
You may qualify if you:
- have no breast cancer symptoms
- have no personal history of breast cancer
- have not had a mastectomy
- have not had a screening mammogram within the last 11 months
- (if transfeminine) have used feminizing hormones for at least five years in a row
If you are considered high risk, talk to your health care provider about your screening options.
What if I’m under 40 or over 74?
If you’re outside the OBSP age range, speak with your health care provider about your risk factors and whether screening is right for you.
Do I need a doctor’s referral for a mammogram?
If you’re between 40 and 74 and at average risk, you can book your own OBSP appointment without a referral.
How much does breast screening cost?
There is no cost for eligible individuals with a valid OHIP card.
How often should I be screened?
For those at average risk, a mammogram every two years is recommended. If you are high risk, you may need to be screened more often – your health care provider can provide you with more information.
How do I know if I’m due for a mammogram?
If you’ve screened before, you’ll receive a letter reminding you that it’s time to book again. If you think you might be due, you can call your nearest OBSP location to find out.
Where can I get a mammogram in Northwestern Ontario?
There are OBSP screening sites in Thunder Bay, Fort Frances, Kenora, and Sioux Lookout. The Screen for Life Coach, a mobile cancer screening bus, also visits rural, remote, and Indigenous communities throughout the region.
Can I get a mammogram if I have breast implants?
Yes. Technologists are trained to work with implants and use special techniques to ensure clear images.
What should I do to prepare for a mammogram?
Wear a loose-fitting top that buttons in the front. Avoid deodorants, antiperspirants, lotions, or powders on your chest or underarms the day of your mammogram, as they can interfere with imaging.
What happens if my mammogram shows something abnormal?
You may be called back for more tests, such as another mammogram, an ultrasound, or a biopsy, to get a clearer picture.
If you still have questions, your health care provider or nearest OBSP location can help. If you’re eligible, take that next step and book your mammogram. To learn more about where and how to book a mammogram nearest you, visit tbrhsc.net/breast-cancer-screening.
Registered respiratory therapists (RRTs) are highly skilled health care professionals with specialized expertise in the assessment, treatment, and management of patients with breathing and cardiopulmonary conditions. They play a crucial role in helping patients breathe easier and recover safely through their advanced knowledge and compassionate care.
At Thunder Bay Regional Health Sciences Centre (TBRHSC), RTs are hard at work 24 hours a day, seven days a week, caring for patients of all ages across every area of the Hospital. From the Intensive Care Unit and Emergency Department to the Operating Room, NICU, outpatient clinics, and even home care, RTs are an essential part of every team.
They respond to high-risk deliveries, traumas, and medical emergencies, provide support during conscious sedations and cardioversions, perform arterial blood gases and catheter insertions, and manage therapies such as non-invasive ventilation (CPAP/BiPAP) and high-flow oxygen. Their dedication and expertise help ensure the best possible outcomes for every patient, every time.
Leadership Roles for RTs

(L-R) Jennifer Gadioma, Interprofessional Educator, and Bruno Tassone, Critical Care and Respiratory Services Coordinator.
Respiratory therapists use their skills and knowledge to take on various leadership roles throughout our Hospital. Darolyn Hryciw is the RRT Charge and her role consists of managing day-to-day operations, scheduling, and equipment and supplies management. Bruno Tassone is the Critical Care and Respiratory Services Coordinator. He is responsible for the day-to-day operations of the Respiratory Care department, Regional Critical Care Response (RCCR) as well as the Medical Emergency Team. Jennifer Gadioma is an Interprofessional Educator. Within her role, she helps advance the practice of health care professionals’ organization wide by providing hospital-wide education. Shawn Jacobson is the Education Lead and he organizes all the education and clinical placements for the Respiratory Therapy students from Canadore College. Aaron Giba is the Professional Practice Lead for the Respiratory department, and provides leadership and guidance in everyday practice as well as policy development and implementation.
Operating Room

(L-R): Brittney Goral RRT and AA; Natalie Pyke RRT and AA; Sam Nigro RRT and AA.
The anesthesia assistant (AA) is an essential member of the Operating Room (OR) team. AAs are respiratory therapists who have an additional 18 months of training in advanced anesthesia skills in order to facilitate the administration of anesthetic services, both in an out of the OR. Within the OR, they assist with the setup and induction of anesthesia for more complex surgical cases. Their duties include advanced airway management, line insertion as well as assistance with epidural/spinal blocks, peripheral nerve blocks and difficult intubation protocols. AAs can prepare and administer a variety of anesthetic agents and manage stable patients under anesthesia while the anesthetist performs other duties within the OR. They also maintain and troubleshoot all anesthesia equipment and are often called upon to assist with anesthetic emergencies. They prepare the OR for malignant hyperthermia cases and are well-versed in the management of this rare but life-threatening emergency. Outside of the OR, AAs set up and assist with sedation cases in diagnostic imaging that require advanced monitoring and generally facilitate any off-service anesthetic duty. The introduction of AAs have allowed anesthesia services to expand at a time when anesthesia resources are very limited.
Outpatient Clinics, Stress lab, Pulmonary Function Testing Lab

(L-R): Loriana Manion, RRT (Stress Lab), and Dennis Poulin, RRT (PFT lab).
Our Respiratory Therapy team plays a vital role across several specialized areas, including the Stress Lab, Pulmonary Function Lab, and Outpatient Clinic. In the Stress Lab, they monitor patients during exercise or pharmacologic stress tests to evaluate how the heart and lungs perform under pressure, helping diagnose conditions like exercise-induced asthma or cardiac issues. In the Pulmonary Function Lab, RTs perform a range of lung function tests such as spirometry and lung volume measurements to assess breathing capacity and identify respiratory diseases like COPD and asthma. Meanwhile, in the Outpatient Clinic, respiratory therapists provide ongoing care and education for patients managing chronic respiratory conditions, ensuring they understand their treatments and maintain optimal lung health outside the hospital setting. Together, these services allow RTs to deliver comprehensive respiratory care that supports diagnosis, treatment, and long-term management.
Paediatric Emergency Transport Team

(L-R): Victoria Morabito, RRT and Taylor Dewal, RRT.
Respiratory therapists on our Paediatric Emergency Transport Team are the critical link between bedside and destination, ensuring patients receive expert respiratory care every step of the way. Whether traveling by ground or air, these skilled clinicians manage ventilators, secure airways, and monitor patients with precision and calm under pressure. Their expertise allows for seamless, safe transitions for our most vulnerable patients — infants and children — often in the most challenging environments. This Respiratory Therapy Week, we recognize our transport RTs for their dedication, adaptability, and commitment to excellence. Their work doesn’t stop at the hospital doors—it’s on the move, saving lives wherever they’re needed most.
For more than 15 years, Angela’s days at the Northwest Regional Cancer Centre were filled with compassion. As a cancer nurse, she supported patients through the hardest moments of their lives.
“I’d tell them to take it one step at a time, and remember they’re not alone,” she says.
Like many others, Angela kept up with cancer screening and tried to live a healthy lifestyle. When she got a letter in the mail reminding her she was due for a routine mammogram with the Ontario Breast Screening Program (OBSP), she booked her appointment with a colleague. Shortly after, Angela was diagnosed with breast cancer.
“I didn’t have any risk factors. I always thought ‘I’m such a healthy person, I don’t have a family history – there’s no way I’m going to get cancer,’” she explains, “And then I did.”
Her experience as a patient was both humbling and transformative. “I knew the treatments, the side effects, the medical side of things. I had never truly understood the emotional weight until I lived it,” she recalls. “I felt very vulnerable.”
Throughout her treatment, Angela stayed active and leaned on the same support systems she once encouraged her patients to rely on. Her family and friends carried her through the hardest days. Her colleagues at the Cancer Centre became her champions.
“I’m used to being independent, so learning to accept help was difficult,” she says. “It also showed me how powerful community can be.”
Today, Angela is cancer-free. She’s back to enjoying travel, with her most recent trip taking her to Europe with friends including nurses from the Cancer Centre. She’s also heading into her fourth year as a nurse on the Screen for Life Coach, a mobile screening bus that brings breast, cervical, and colon cancer screening services to communities across Northwestern Ontario.
“My breast cancer was found early because I stayed on top of my mammograms,” Angela shares. “It feels good to be part of bringing that same opportunity to others, especially in communities where accessing these services can be challenging.”
On the Coach, Angela meets people where they are: in their own communities, surrounded by their own support systems. For her, it feels deeply personal.
“I understand now that the smallest gestures can make the biggest difference,” says Angela. “Kindness goes a long way especially when people are feeling anxious. Creating a connection is important, and now I can look someone in the eye and say, ‘I’ve been where you are.’”
This Breast Cancer Awareness Month, speak to your primary care provider to see if breast cancer screening is right for you. The OBSP recommends that most eligible women, Two-Spirit, trans and non-binary people ages 40 to 74 get screened with mammography every two years. A referral from a primary care provider is not required for individuals at average risk.
For more information about breast cancer screening, visit tbrhsc.net/breast-cancer-screening.
One in nine women in Ontario will face breast cancer in their lifetime, with many diagnosed before turning 50. Now, thanks to a recent expansion of the Ontario Breast Screening Program (OBSP), people in their 40s no longer have to wait to be screened. The province’s decision to lower the self-referral age from 50 to 40 gives approximately one million additional women, trans, and non-binary people across Ontario the chance to be screened earlier.
“Breast cancer can and does occur in people in their 40s,” says Dr. Nicole Zavagnin, Regional Primary Care Lead for Cancer Care Ontario at Thunder Bay Regional Health Sciences Centre. “Having the option to begin screening earlier means more people can be diagnosed at an earlier stage, when treatment is more effective.”
Through the OBSP, eligible individuals aged 40 to 74 who are at average risk can book a mammogram every two years at no cost with a valid OHIP card – no doctor’s referral needed. Those at higher risk, such as those with a family history of breast cancer, may need to start screening earlier or be screened more often based on advice from their healthcare provider.
Mammograms remain the most reliable tool for breast cancer screening, able to detect changes in breast tissue before symptoms appear. The benefits are clear: the five-year survival rate for breast cancer found at stage 1 is nearly 100%, but drops to less than 30% when diagnosed at stage 4.
“Cancer screening is for people who feel well and haven’t noticed any changes,” days Dr. Zavagnin. “By expanding eligibility, more patients can benefit from early detection and the wider range of treatment options it allows.”
While mammograms are key to early detection, breast health also involves knowing your body, reporting changes promptly, and maintaining a healthy lifestyle.
“Breast Cancer Awareness Month is a great time to reflect on your personal risk factors and talk with your healthcare provider about whether screening is right for you,” notes Dr. Zavagnin.
Where to Get Screened in Northwestern Ontario
Thunder Bay
Linda Buchan Centre for Breast Screening and Assessment, TBRHSC
980 Oliver Road
(807) 684-7777
Thunder Bay Diagnostics
63 Algoma St. N, Suite 100
(807) 683-4411
Screen for Life Coach (serving Thunder Bay and regional communities)
(807) 684-7777
Fort Frances
Riverside Health Care Facilities
110 Victoria Avenue
(807) 274-4808
Kenora
Lake of the Woods District Hospital
21 West Sylvan Street
(807) 684-7777
Sioux Lookout
Sioux Lookout Meno Ya Win Health Centre
1 Meno Ya Win Way
(807) 737-6579
To learn more about breast cancer screening, visit tbrhsc.net/breast-cancer-screening.
Thunder Bay Regional Health Sciences Centre (TBRHSC) is excited to welcome the public to its Open Doors Career Showcase on Wednesday, October 8, 2025, from 6:00 p.m. to 9:00 p.m. The event will be held in the Hospital’s Cafeteria at 980 Oliver Road.
This interactive, in-person event offers a unique opportunity to discover the wide variety of career paths available across all departments and professions at TBRHSC. Attendees will have the chance to engage directly with health care professionals, participate in guided tours of key Hospital departments, and connect with representatives from local educational institutions.
Whether you’re a high school student considering post-secondary options, a college or university student exploring career pathways, a working professional looking for a change, or someone without formal education seeking direction, this event is designed with you in mind.
“Experiencing the health care environment firsthand helps people truly understand the wide range of roles available,” says Jeannine Verdenik, Vice President, People and Culture at TBRHSC. “This event opens doors — literally and figuratively — for individuals to discover career options they may never have considered. Whether your interests are clinical, technical, or administrative, there’s a place for you in health care. We encourage anyone curious about their future to attend and find out why our Hospital is a place to work, grow, and thrive.”
There is no cost to attend, and complimentary parking is available for all attendees in Lot G, located near the East/Cafeteria entrance. Those interested in learning more about the event, or about a career in health care are asked to contact the Human Resources team at TBRHSC via email at TBRHSC.HumanResources@tbh.net or by calling (807) 684-6227.
(Originally published in the October edition of Health System News)
Stroke remains one of the leading causes of death and disability in Canada, disproportionately affecting older adults. The key to reducing the impact of stroke is rapid recognition and immediate action. Yet too often, warning signs are missed, delaying treatment and reducing the chances of recovery.
Thunder Bay Regional Health Sciences Centre’s Northwestern Ontario Regional Stroke Network has been leading the FAST Heroes campaign since 2019. FAST Heroes is an innovative, school-based health education stroke awareness program that bridges generations by engaging children to share lifesaving knowledge with their grandparents. Developed internationally with endorsement from the World Stroke Organization and gaining momentum in Canada, FAST Heroes turns primary grade students into ambassadors of stroke awareness, teaching them to recognize the signs of stroke summarized by the acronym FAST: Face, Arms, Speech, and Time, time to call 9-1-1.
But the impact goes beyond education. The program directly advances hospital mandates to the community, particularly for older adults. Grandparents are the primary target audience of this initiative; by equipping them (through their grandchildren) with the ability to identify the early warning signs of stroke, hospitals and health systems can help ensure that older adults receive the right care, in the right place, at the right time.
Ontario hospitals are increasingly focused on developing care models that prioritize prevention, integration, and partnership with families. While advanced stroke units, telestroke networks, and rehabilitation services remain critical, earlier activation of emergency care remains the single most effective way to improve outcomes. FAST Heroes Canada received endorsement from the Ontario Association of Paramedic Chiefs, in which all EMS services across Ontario are able to support this program through classroom engagement.
The FAST Heroes model contributes to a new way of caring for older adults by:
- Empowering families: Children become health champions, fostering intergenerational learning within households.
- Promoting timely care-seeking: Older adults who internalize FAST are more likely to activate emergency services immediately, arriving at stroke-ready hospitals within the treatment window.
- Strengthening community-hospital connections: Stroke Networks across Ontario are continuing to endorsing FAST Heroes and exploring ways to integrate this awareness campaigns into their community outreach. Staff become FAST Heroes ambassadors and collaborate with school boards and schools to incorporate FAST Heroes into the primary educational settings. Evaluations show that children not only learn and retain the information but are eager to share it with their grandparents, multiplying the program’s reach.
These kinds of initiatives represent an important stride in caring for older adults. By meeting patients and families outside of hospital settings, health systems can help reduce stroke-related disability, preserve independence for seniors, and lessen the long-term burden on hospitals and long-term care facilities.
As Ontario hospitals continue to reimagine services for our aging population, the FAST Heroes program is a strong example of how creative partnerships and community education can complement traditional models of care. By empowering the next generation to safeguard their grandparents’ health, we are not only raising stroke awareness but also building a culture of shared responsibility that ensures older adults receive timely, lifesaving care.
Those interested in learning more about FAST Heroes can visit www.fastheroes.com, or contact Keli Cristofaro at Keli.Cristofaro@tbh.net or Canadaheroes@fastheroes.org.
In 2012, Connie Gray-McKay received a letter from the Ontario Breast Screening Program (OBSP) inviting her to book a mammogram. At the time, she was a busy mother and Chief of Mishkeegogamang First Nation, and admits that personal health appointments were not her first priority.
“When that first letter came, and the ones after it, I just put them aside,” Connie recalls. “There were always other responsibilities. Getting to a screening appointment outside the community wasn’t easy, and it didn’t feel urgent at the time.”
Life moved quickly, until five years later in June 2017. Sitting on her couch, reviewing the Chief nomination forms and debating whether to run for re-election, Connie felt a lump.
“Within a couple of days I was sent to Sioux Lookout Meno Ya Win Health Centre for a mammogram, followed by a biopsy a week later,” she says. By early July, she was diagnosed with breast cancer.
Connie’s story reflects a broader reality in Northwestern Ontario, where access to cancer screening can be challenging. For many remote, rural and Indigenous communities, travel, scheduling, and limited availability of healthcare providers often stand in the way of timely appointments.
To help bridge those gaps, the Screen for Life Coach (Coach), a mobile cancer screening bus, hits the road each year for a seven-month regional tour. The Coach delivers breast, cervical, and colon cancer screening services directly to communities in Northwestern Ontario where these services may otherwise be limited or non-existent.
“Improving access to cancer screening is our goal. By bringing services closer to home and providing culturally safe care, it’s easier for individuals to prioritize their health and detect cancer early, when treatment works best,” explains Tarja Heiskanen, Manager of Prevention and Screening Clinical Servicesat Thunder Bay Regional Health Sciences Centre. “This travel season, we’re proud to say we’re on-track to screen 14 Indigenous communities in Northwestern Ontario.”
Recent updates to Ontario’s screening programs are further expanding access and opportunity. “Last fall, the Ontario Breast Screening Program lowered the recommended starting age for breast screening mammograms from 50 to 40,” says Heiskanen. “opening the program to many more people who could benefit from early detection.”
Colon cancer screening is also becoming more accessible through the FIT Kits-on-Hand initiative. Building on its success in the Sioux Lookout area, the program launched in the Treaty #3 territory in July 2025. Now, eligible individuals in participating communities can pick up a Fecal Immunochemical Test (FIT) from their local nursing station rather than waiting for it to arrive by mail.
“FITs are convenient and can be completed entirely at home,” Heiskanen adds. “This means people can take the test without leaving their community. Time is of the essence when it comes to screening, so reducing wait time is very important when considering potential outcomes.”
Stories like Connie Gray-McKay’s highlight why timely access to screening matters. For Connie, her breast cancer diagnosis marked a turning point. She chose not to run for Chief again so she could focus on her health and family. Now cancer-free, Connie uses her voice to encourage other Indigenous people to put screening first, even when life feels busy or travel feels overwhelming.
“In our communities, we are used to putting others first: our families, our Elders, our children. But screening is how we take care of ourselves so that we can stay present for our loved ones,” she says.
This Breast Cancer Awareness Month, Connie’s message is simple but powerful: “Don’t wait. Cancer doesn’t care how busy you are. Screening gives us a fighting chance, and our people deserve that chance.”
For information on cancer screening in Northwestern Ontario, as well as the Coach’s current regional and Thunder Bay schedules, visit tbrhsc.net/cancerscreening. Planning for the Coach’s 2026 travel season is currently underway.
Who should get screened
In Ontario, the cancer screening guidelines for average risk individuals are as follows:
- Breast cancer: Women, Two-Spirit, trans and non-binary people between the ages of 40 and 74 should have a breast screening mammogram every two years.
- Cervical cancer: Anyone with a cervix between 25 and 69 years, who has ever been sexually active, should have a cervical screening test every five years.
- Colon cancer: Individuals, between the ages of 50 and 74, who have no first-degree family history of colon cancer, should complete a take-home colon screening kit every two years.
Cancer screening is available at no cost for those with a valid OHIP card. A doctor referral is not required for average-risk individuals within the recommended screening age range.
As cold and flu season approaches, we want to remind the community that in the event of an increase in respiratory-related illnesses, our Hospital is prepared to enhance safety protocols to help protect patients, families, and staff.
Masks are available at all public entrances on our sanitizing stands, and hand sanitizer dispensers are located throughout the Hospital. We encourage everyone to use these resources to help reduce the spread of illness.
Our Infection Prevention and Control team continues to monitor infection trends closely. Any updates to masking requirements or other safety measures will be communicated clearly and promptly.
If you are feeling unwell and have an appointment, please contact the reception desk in advance to discuss your visit. If you are planning to visit someone on an inpatient unit, we kindly ask that you postpone your visit until you are feeling better.
Thank you for your continued cooperation in helping us keep our Hospital and community safe.
Welcome back. I hope that you had the opportunity to enjoy a restful and rejuvenating summer break. Fall brings with it new opportunities and renewed momentum, and I’m confident that together with staff, professional staff, learners and volunteers, we will continue to advance the goals of our Hospital and the health of the communities we serve.
As the Board reconvenes, I would like to express my sincere appreciation for our board members continued commitment to the governance and strategic oversight of our institution. Before the summer break, our Hospital celebrated another successful year at the Annual Meeting of the Corporation in June. I’m pleased to announce the return of Christine Bates, Charles Campbell, Dr. Andrew Dean, Kimberly Ferris, Michael Pelletier, James Peotto, Matt Simeoni, Joy Wakefield, and Gord Wickham to the Thunder Bay Regional Health Sciences Centre’s Board. Joining as new members are Matthew Aiken and Marla Morrison. Jesse Fiddler was appointed to a two-year term as the new Community Member on the Resource Planning Committee.
We bid farewell to Douglas Judson who, during his two terms with the Board of Directors honoured us with his passion and dedication to the Hospital and to the region.
The Board includes the ex-officio Directors Dr. Rhonda Crocker Ellacott, President and CEO; Dr. Armour Boake, President, Professional Staff Association; Dr. Michael Green, Dean, President and CEO, NOSM University; Dr. Bradley Jacobson, Chief of Staff; and Adam Vinet, Chief Nursing Executive.
Over the summer, the Hospital officially broke ground on construction for its new Cardiovascular Surgery Program. Hospital staff, health care partners, community donors, and government representatives were onsite to recognize this long-anticipated moment and to celebrate the beginning of construction of more than 76,000 square feet of new and renovated clinical space. This program is the first of its kind in Northwestern Ontario and is being developed in partnership with University Health Network’s Peter Munk Cardiac Centre to ensure the highest standards of care. When complete, the program will include 14 new cardiovascular surgery inpatient beds. This marks a major step forward in providing access to life-saving care for people in the region.
With the new season upon us, the recently released 2024-25 Annual Report outlines the progress achieved over the past year as we continue to advance the Hospital’s Strategic Plan 2026. This year, a video highlighting the strategic priority Patient Experience demonstrates our ongoing commitment to delivering compassionate, patient-centred, and high-quality care that reflects the diverse needs of patients and families across Northwestern Ontario.
Throughout September our Hospital’s Indigenous Collaboration, Equity and Inclusion portfolio organized many events to honour residential school survivors and to underscore the importance of Truth and Reconciliation. Events included displaying the Nishnawbe Aski Nation Community panels, a beading opportunity for staff, and an educational session with Elder and Residential School Survivor Peter Sackaney. As part of our commitment to Truth and Reconciliation, and the 94 Calls to Action, our Hospital also published our second annual report outlining the past year’s progress on the Calls to Action and our next steps. We remain committed to promoting transparency in our Calls to Action and to continue to work towards creating an environment of inclusion, equity and compassion at our Hospital.
This month will mark 16 years of Sharing and Caring Together. This a week-long event demonstrating our successes in patient and family-centred care will culminate in an exhibition which displays some of the initiatives developed to continue to deliver the highest quality of care to patients and families. It is truly incredible to witness the dedication and commitment of our staff as they continue to improve the patient and family experience.
In addition, this month is the annual Luncheon of Hope, a fundraising event hosted by the Thunder Bay Regional Health Sciences Foundation in support of advancing care for patients with breast cancer. The funds raised at this annual event enables our Hospital to purchase state-ofthe-art equipment to provide exceptional diagnostic services and care for our patients who are fighting breast cancer and their families. I would like to express my gratitude to the Foundation for organizing the event and to the sponsors and donors for their attendance and support. Through these events, we continue to expand on the latest diagnostic and treatment options for the many patients who need quality cancer care close to home.