Compre-
hensive
Clinical Care
Enhance the delivery of our clinical services.
Comprehensive Clinical CareThunder Bay Regional Health Sciences Centre
Our Vision
healthy
together
Our Mission
We will deliver a quality patient experience in an academic health care environment that is responsive to the needs of the population of Northwestern Ontario.
Our Philosophy
Patient and Family Centred Care is the philosophy that guides us. Patients and Families are at the centre of everything we do.
We will focus our efforts on Patient Experience, Seniors' Health, Comprehensive Clinical Care, Aboriginal Health and Acute Mental Health.
Our Values
Patients ARE First:
Patients and families at the centre of everything we do. At our acute health care facility, we provide care to the people of Northwestern Ontario - a region the size of France.
Ours is the teaching hospital of choice for over 1,500 learners from the Northern Ontario School of Medicine, Lakehead University, Confederation College, and other partnering academic institutions. We are an academic health sciences centre, committed to teaching the next generation of health care providers and advancing medical research. Patients benefit from interprofessional teams of healthcare providers and access to leading-edge medical equipment and clinical trials.
Providing effective health care for patients and families has earned us both Innovation Awards and Leading Practice Designations. We are a national leader in Patient and Family Centred Care.
The Health Sciences Centre belongs to the community it serves; the 250,000 residents of Northwestern Ontario. Our Strategic Plan 2020 was built by and for them.
We are pleased to provide this report on the 2016-2017 fiscal year progress of the Strategic Plan 2020.
Leader Messages
Message from the Chair of the Board of Directors

We have now completed two years of our five-year Strategic Plan 2020 and I’m so pleased with the progress we’ve made. Our Patient and Family Centred Care (PFCC) philosophy guides us in all of initiatives. It fosters transformation of our organization for the better to enhance patients’ outcomes, their families’ integration in our care teams and our staff and physician engagement at their bedside.
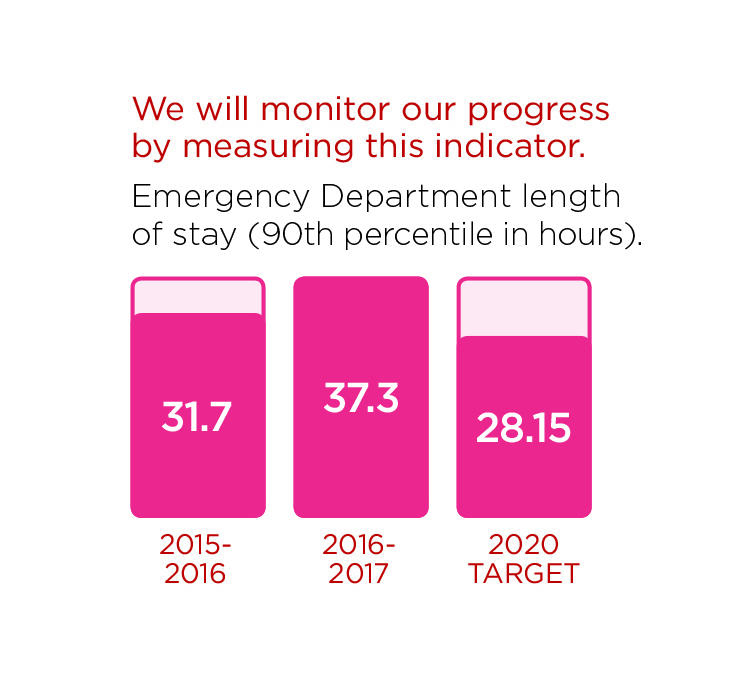
We are grateful for our 5 Partners’ ongoing input on strategies that help us further improve patient care. Our latest 5 Partner engagement session on June 7th focused on our five Strategic Directions: Patient Experience, Comprehensive Clinical Care, Seniors’ Health, Indigenous Health and Acute Mental Health. We also grateful for our partners’ collaboration to improve patient flow, particularly in our Emergency Department.
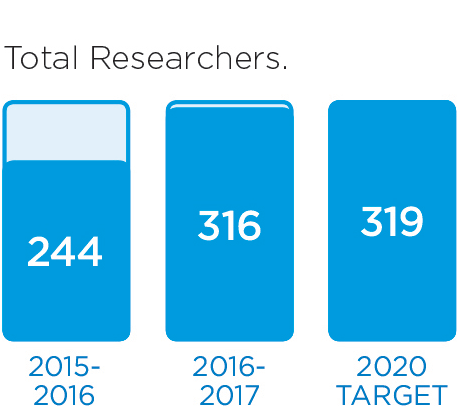
Our much valued research arm, the Thunder Bay Regional Health Research Institute is also helping us reach our goals. Our scientists cooperate closely with clinicians, medical professionals, as well as academic and industry partners to improve health care through excellence in patient-centred research. Their research allows us to better understand our priorities, which not only leads to better outcomes for our patients and their families, but to efficiencies that ultimately improve our bottom line.
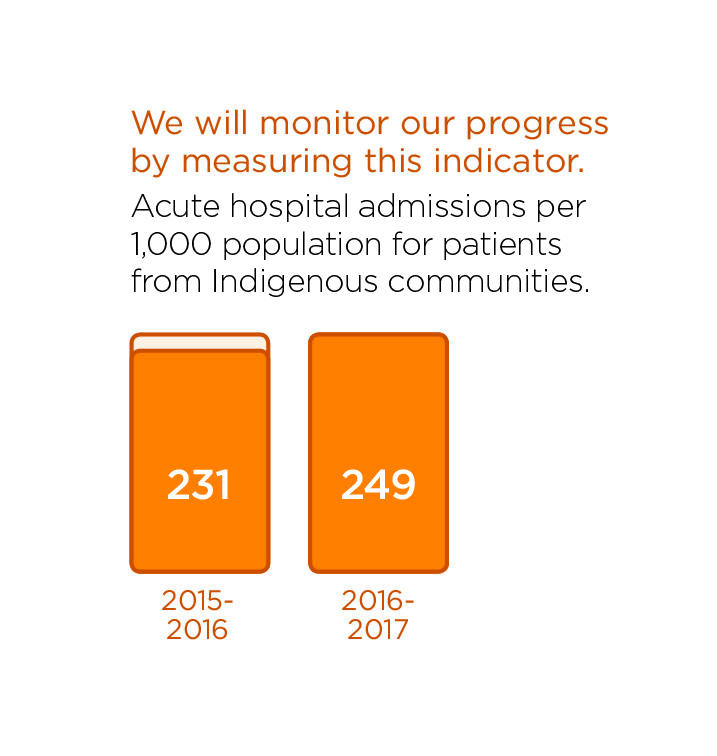
One of the shared priorities of our hospital and Health Research Institute is improving Indigenous Health disparities. Geographical isolation and socio-economic disadvantages contribute to the health disparities faced by the 69 Indigenous communities we serve. Our scientists and clinicians are connecting with Indigenous communities and their leaders to determine how we can better address their health needs and expectations.
I am impressed by our exceptional staff, physicians, scientists and volunteers. Their commitment to consistently providing quality health care in persistent clinical challenges is inspiring. Day after day they work together to deliver on our Mission and advance our Strategic Directions as their priority. It is humbling to serve alongside such skilled, dedicated and engaged health professionals and workers.
I take this opportunity to recognize Board Directors who are completing their terms with us today. I am so grateful to have had the opportunity to get to know and be inspired by Doug Shanks, Gerry Munt and Georjann Morriseau. Thank you for all you have done for patients and their families through your leadership as Board Directors. In recognition of your role, we have donated $500 in honour of each of you to the Northern Ontario School of Medicine bursary fund. Again, thank you for your contributions. You will be missed.
I invite you to read through our 2016-17 Annual Report where you will learn more about some of our significant accomplishments of the last fiscal year.
Thunder Bay Regional Health Sciences Centre serves you, the residents of Northwestern Ontario. Our dedicated Board of Directors are committed to serving you as we advance our vision, Healthy Together.
Thank you.
Nadine Doucette
Chair, Board of Directors
Message from the President and CEO

I am pleased to say that we have seen incredible successes again this year. Guided by our Strategic Plan 2020 and its five Strategic Directions (Patient Experience, Comprehensive Clinical Care, Seniors' Health, Indigenous Health, and Acute Mental Health), we improved patient care throughout the hospital. Our 5 Partners in Health – members of the community, policy makers, health managers, representatives of academic institutions, and health professionals – helped us keep on track and re-evaluate our goals.
One of the most exciting milestones this year was our first endovascular aneurysm repair (EVAR). Providing advanced and life-saving cardiovascular surgical procedures such as EVAR will significantly reduce travel, stress, and the risk of complications for our critically ill patients.
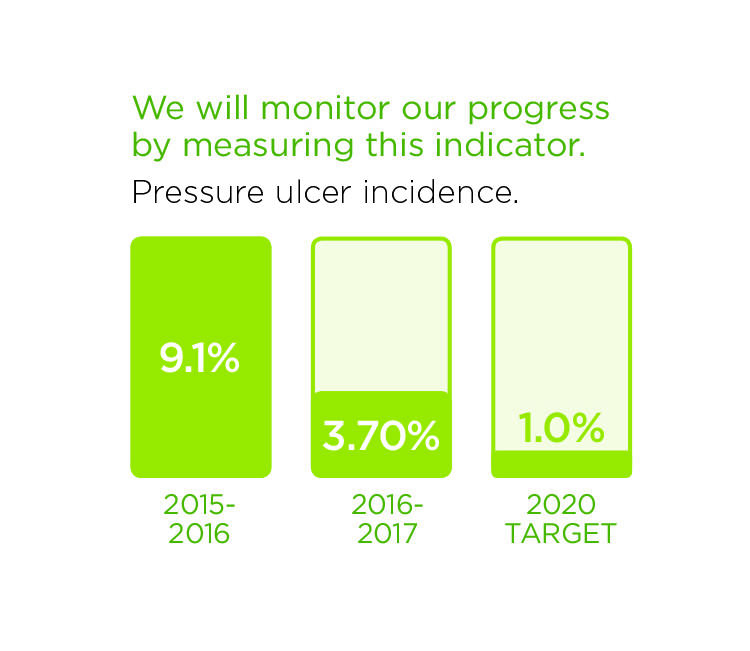
In Senior's Health, new practices will reduce the incidence of pressure ulcers, and a nurse-driven training program called Nurses Improving Care for Health System Elders is tailoring our services to accommodate the specific needs of our senior patients.
We are implementing a new mental health screening tool that will screen inpatients who may be struggling with mental health issues. This will allow us to keep these patients safer while being treated in a medical unit by identifying potential hazards.
In Indigenous Health, we launched new resources to support patients returning to their remote communities to improve self-management, access to care, and the patient care experience as they transition home. We continue to strive to make the hospital environment more welcoming by encouraging staff and volunteers to take Ojibwe language lessons, offered free of charge.
One initiative that is not as visible is our new "Me to We to All" leadership concept. Designed to improve employee satisfaction – and in turn patient care – this approach will create a more collaborative environment with leaders who focus on teamwork.
Under the leadership of Dr. David Puskas and Director Caroline Fanti, the Regional Orthopaedic Program gained tremendous momentum in the past year. The integrated regional program will provide close-to-home orthopaedic care, with regional sites in Fort Frances, Kenora and Dryden offering surgery, consultation and support.
You'll read about these initiatives and more in this Annual Report.
In addition to advancing the priorities identified in our Strategic Plan 2020, we also experienced several significant operational successes. One is our continued improvement in patient flow. Collaboration with systems partners, combined with the extraordinary efforts of staff and physicians, translated in 2016-17 fiscal year to 61% days in surge capacity. This is down significantly from 72% the previous year, and 92% in 2014-15. Our average length of stay has also improved to 5.31 days, compared to 5.66 last fiscal year and 5.85 the year prior.
Our anticipated $6.9 million deficit for 2016/17 was reduced to less than $0.5 million as a result of performance improvements and one-time funding from the North West LHIN.
We welcomed two new members to our Senior Leadership Team. Amanda Björn, Vice President, Human Resources, brings experience in organizational development, planning, implementation, monitoring and evaluation of corporate educational and people development services as they relate to the organization’s Vision and Strategic Plan. Dr. Abraham (Rami) Rudnick, Vice President, Research (for the Hospital) and Chief Scientist (for the Health Research Institute) offers a wealth of experience from many years in leading interprofessional health research as well as developing and supporting research.
I would also like to highlight that research at our Hospital and our research arm, the Thunder Bay Regional Health Research Institute, is growing steadily. The number of people participating in clinical trials is increasing, and clinical research in several health disciplines is expanding. In particular, Indigenous Health research is prioritized as a central focus of our new Strategic Plan. As well, our basic science is making headways, with clinically applicable innovations in HP gas MRI, high-intensity focused ultrasound (HIFU), and cell biology, among others. Finally, our cyclotron facility has started producing radioisotopes that are used now to calibrate our positron emission tomography (PET) equipment. We have submitted application to Health Canada for licencing to produce isotopes to be used with our patients in the coming months.
None of these successes would be possible without our staff and physicians. Their commitment to continually improve and enhance the care we provide is vital to meeting our goals. I commend them all for their compassion and their dedication to Patient and Family Centred Care (PFCC). You make this an organization that we can all be proud of.
Thank you.
Jean Bartkowiak

President & CEO
Message from the Co-Chair, Patient and Family Advisory Council

Once again, the last twelve months have sped by. It’s hard to believe that it's been eight years since we fully embraced Patient and Family Centred Care (PFCC) and have been integrating the voice of the patient and their families into everything we do.
I am proud of our leaders, staff and volunteers for remaining so committed to our PFCC philosophy. I’m also proud to report that our group of nearly 100 Patient Family Advisors (PFAs) has stayed busier than ever working on hundreds of committees that address issues and policies such as visiting hours, parking, and menu choices. We’ve also been working on clinical policies and practices across the entire spectrum of services offered at our Hospital.
We have built a reputation as leaders in Patient and Family Centred Care. Before we do anything, we ensure that PFAs are consulted and the patient’s voice is heard. This way of thinking is embedded in our corporate culture and we wouldn’t have it any other way.
More and more hospitals across Ontario, and the country, are beginning to adopt the PFCC philosophy. In fact, it is so successful and impactful that the Ministry of Health and Long-Term Care now requires that all hospitals integrate the patients’ voice in all aspects of care. I take pride in the knowledge that we were doing this long before it was required.
I speak for my fellow PFAs when I say we are honoured to be part of the team at Thunder Bay Regional Health Sciences Centre. The staff, leadership and volunteers are phenomenal. As a team, we share our common goal to be Healthy Together, and together, we are making it happen.
Thank you.

Co-Chair, Patient and Family Advisory Council
Message from the Medical Advisory Committee

Throughout the year, the Medical Advisory Committee guides quality medical care, health education programs, health research and patient safety. This ensures that Thunder Bay Regional Health Sciences Centre remains a leader in Patient and Family Centred Care (PFCC).
This past year, our focus has been to develop a Quality Health Care Framework to address the Hospital’s 2020 Strategic Direction, to enhance the quality of the patient experience. We recognize that the contributions of staff, learners, physicians, patients, and patient family advisors are essential in achieving quality health care. The Framework extends on the core concepts of our PFCC philosophy beyond patients to include all people. It guides and focuses our efforts to deliver high quality health care and achieve measurable improvements. Through a shared understanding of our common goals, every member of our Hospital team contributes to health care that is safe, effective, patient and family centred, efficient, timely, and equitable.
Our organization has committed to developing physician leadership to enhance and help lead system transformation. The sustainability of our health care system relies heavily on physician engagement, as well as physician leadership. This will ensure that the proper focus is on continuous quality improvement and quality and safety within our organization. All physicians at our Hospital are responsible for and committed to quality care. We have enhanced efforts to engage physicians as partners in our Strategic Plan 2020, and their dedicated efforts have contributed to improvements in Average Lengths of Stay.
Physician engagement will be further required as we embark on trying to develop a standardized communication strategy for Professional Staff. We anticipate that by learning how to effectively communicate information that is vital to Professional Staff practice will enhance their involvement in standardized quality and safety initiatives. We are also committed to ongoing engagement to support physician satisfaction, which in turn enhances patient experiences.
Finally, the Medical Advisory Committee and Dr. Stewart Kennedy, Executive Vice President, Medical and Academic Affairs are developing an integrated leadership development model with Northern Ontario School of Medicine, Thunder Bay Regional Health Sciences Centre and Health Sciences North. The ultimate goal is to build the culture of academic and research integrated in departmental and clinical obligations centered on quality and safety.
In the fast-paced and ever-changing health care environment, it’s important that we continue to evolve along with it. I’m proud to be part of an academic health sciences centre that fosters an environment of innovation and learning, and always strives to improve the quality of the patient experience.
Thank you
Dr. Gordon Porter

Chief of Staff
Chair, Medical Advisory Committee
Patient Experience
We are leaders in Patient and Family Centred Care (PFCC), and it is the philosophy that guides us. We recognize that creating a quality patient experience builds upon this philosophy.
We are focused on enhancing the Patient Experience as one of our strategic priorities. Our goals are to:
- Develop a framework to deliver high quality care;
- Enhance understanding and continue to grow and embed our PFCC philosophy;
- Advance the academic environment;
- Invest in staff development, engagement and wellness;
- Use information technology to advance the patient experience.
We will know we are successful by 2020 when we demonstrate:
- No harmful events;
- Patients are highly satisfied & engaged in care;
- A research culture;
- Learners are satisfied;
- Staff and physicians are engaged in care;
- Advanced information technology supports patients and care providers.
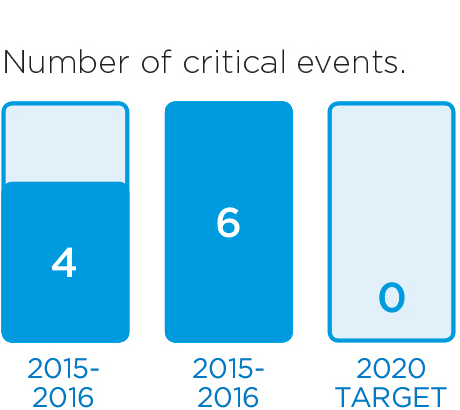
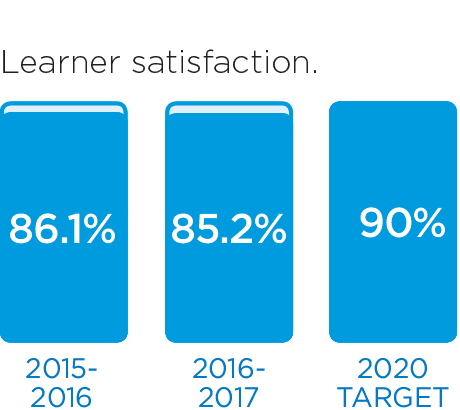
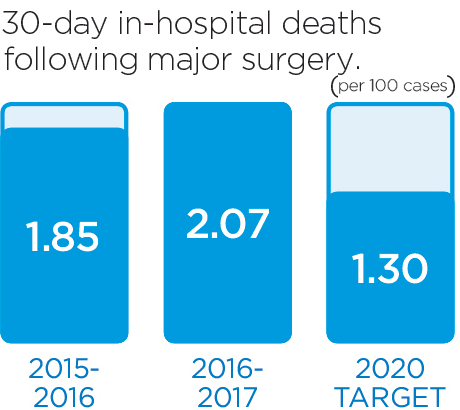
We will monitor our progress by measuring these indicators.
These stories provide an insight into three of the many Patient Experience initiatives in 2016/17:
New Leadership Philosophy to Improve Staff Engagement
An engaged staff helps foster a greater clinical, academic, and scientific environment for our patients and their families at the Health Sciences Centre. Leader rounding provides managers the opportunity to open a constructive dialogue with their teams.
Leaders Provide a Personal Level of Care to Improve the Patient Experience
Patients and families should always expect the best care possible. To ensure those expectations are met, our patient care leaders are engaging in a practice known as “leader rounding on patients”.
New Leadership Approach Will Help Improve Patient Care
A new leadership approach called “Me to We to All” is designed to build upon each leader’s individual strengths, create more collaborative and supportive teams, and ultimately improve patient care.
New Leadership Philosophy to Improve Staff Engagement
An engaged staff helps foster a greater clinical, academic, and scientific environment for our patients and their families at Thunder Bay Regional Health Sciences Centre. When we introduced the new tactic of Leader Rounding, Michele Miller, Manager of Cardio-Respiratory Services, was excited for the opportunity to further connect with her team.
"When leadership rounding was introduced, I was fully on-board and ready to start a more formal approach, having direct questions that I could weave into conversations," said Michele. "It gave me a new reason to reconnect with my team and socialize with a purpose."
Leader Rounding provides managers the opportunity to open a constructive dialogue with their teams about what is working well within their jobs, what could be improved, and what could be done differently. It’s also a great way to recognize employees for a job well done.
"Open communication is so important. Employees need to be comfortable sharing their concerns and opinions and they want to feel like they’re really being heard," said Michele. "As a manager, it’s my job to ensure that my staff have the tools they need to do their work. In order for managers to do that, we need to listen to what we’re being told and keep pursuing those conversations."
Michele believes that Leader Rounding also enables a more proactive approach to improving the work place. "By always checking in and asking how things are going, we can make any necessary changes in a more controlled and positive way, rather than responding to a problem or crisis after it has already occurred," she explained.
Michele has noticed a positive change. "My staff appear happier and more trusting of me and my role as someone who is part of their team, working with them and supporting them in what needs to be done. It’s been really encouraging."
After 29 years at the Health Sciences Centre and 20 years in a leadership role, Michele's biggest take-away lesson is that everything boils down to relationships. "Everyone has a story," she said. “Listen to what your team has to say so that you can be a better leader for them. When everyone works together, we have much better outcomes in terms of employee satisfaction, and that translates to better outcomes for our patients and families."

Michele Miller, Manager of Cardio-Respiratory Services, uses Leader Rounding to further connect with her team. When leaders round on employees, they get to know them better, it shows responsiveness to needs, and allows for an opportunity to recognize great work.
Leaders Provide a Personal Level of Care to Improve the Patient Experience
Adopted as a best practice tactic, leader rounding on patients is when nursing leaders regularly check in with each patient on their unit. It helps reconnect leaders to patient care on a personal level, while enabling our leaders to either recognize good clinical practice or identify and respond to potential gaps in care.
"Leader rounding on patients helps ensure that the absolute best level of care is provided to every patient, every time," said Ron Turner, Senior Director of Patient Services. "By personally interacting with patients and families, our leaders are able to address the patients' expectations and assist in the effectiveness of their treatment. It's also a great opportunity to connect with the patient and their family to address questions and manage potential anxiety. Sharing information about the unit, our staff, training and experiences all help to put a patient’s mind at ease."
Leader rounding is one of the many ways our Hospital is working to enhance the quality of the patient experience, which is a top priority within the Strategic Plan 2020. It allows us to identify further opportunities to improve quality care that is: safe, effective, patient and family centred, timely and accessible, equitable, and efficient.
"Creating a quality patient experience builds upon our Patient and Family Centred Care philosophy (PFCC). Our patients benefit from this practice as it connects our Hospital with our patients and their families and ensures that we are always reevaluating our care, care processes and overall quality experiences," said Turner. "This open dialogue also creates an empathetic connection between our leaders and patients. From there, our leaders are able to proactively assess the quality of our care using direct, focused questions to determine any potential gaps and immediately address concerns."
After rounding on patients', leaders provide feedback to staff that provides recognition for practices that patients identify as making a positive difference, with coaching for staff that is consistent with the behaviors that have been identified as important to patients. This connects immediately back real time to support improvements in care or reinforce excellence in practice.
"So far, this practice has been a great way to demonstrate our commitment to being respectful and responsive to the needs and values of our patients and their families," said Turner. "We listen to their questions, concerns and values, and use that feedback to guide our decisions and practices moving forward so that the experiences of our patients are positive."

Patients and families of Thunder Bay Regional Health Sciences Centre should always expect the best care possible. To ensure those expectations are met, our patient care leaders are engaging in a practice known as “leader rounding on patients”.
New Leadership Approach Will Help Improve Patient Care
A new leadership approach at the Thunder Bay Regional Health Sciences Centre called “Me to We to All” is designed to build upon each leader’s individual strengths, create more collaborative and supportive teams, and ultimately improve patient care.
"We want to create a positive place to work," said Amanda Björn, Vice President of Human Resources. "I believe that the leaders need to care for the people who care for our patients. Happy staff, happy patients."
Björn joined the Health Sciences Centre’s senior leadership team in August 2016. Previously, she worked at Providence Healthcare in Toronto, where she first began developing the approach. She introduced it to approximately 110 directors, managers, coordinators, union leaders, physicians, and other Hospital leaders in spring 2017.
Björn said it's about changing the leadership culture at the Hospital from the top down. "We have to focus on staff-centred leadership as part of Patient and Family Centred Care (PFCC). It’s just as important," she said.
In developing the Me to We to All leadership and organizational development framework, Björn drew from several accepted approaches including the LEADS in a Caring Environment framework. Like other leadership approaches, Me to We to All is a complex and comprehensive approach. One of the main principles is to help leaders understand themselves better.
"Typical leadership training helps you focus on skills such as managing budgets, managing conflict, and so on. For example, conflict management training provides tips and skill-building, but it’s a cookie-cutter approach that doesn’t take into consideration your own natural abilities or even your weaknesses," Björn said.
Me to We to All helps an organization's leaders understand themselves better so that they can enhance leadership skills and a customized leadership approach that will be most effective for them.
"It’s less of a competency approach, and more of a way to discover which approach works best for your strengths and values."
It’s also designed to encourage collaboration rather than command and control and to reduce the rigidity of the typical leadership pyramid that exists in organizations. This is in line with the developing leadership megatrends we are seeing, where managers from C-level executives on down collaborate with and enable others – the "on-the-ground experts" – to make the decisions themselves.
"If you have an organization where everyone is playing politics and they’re not open and vulnerable with each other, that gets in the way of achieving results," Björn said. A more collaborative environment where everyone is working together towards the same goal improves results, reduces stress, and makes for a happier work environment. In turn, that will lead to better patient care.
Another part of this approach is Björn’s "Learning Community" concept. Part conference break-out group and part workshop group, Learning Communities brings together leaders from different parts of the Hospital to learn together, provide support, and bounce ideas off each other. It’s taken directly from the “two heads are better than one” playbook: the idea is to talk through challenges in an open, supportive environment and get feedback.
"Our leaders get support from their peers and opportunities to discuss leadership and new ideas on how to handle situations. We are creating a space where our leaders can gather and grow together."

"We want to create a positive place to work,” said Amanda Björn, Vice President of Human Resources. “I believe that the leaders need to care for the people who care for our patients. Happy staff, happy patients."
Comprehensive Clinical Care
We aim to enhance the Comprehensive Clinical Care that transcends the organization and touches all patients. Our activities are focused on addressing gaps in care, so the people of Northwestern Ontario can receive quality care, closer to home.We aim to enhance the Comprehensive Clinical Care that transcends the organization and touches all patients. Our activities are focused on addressing gaps in care, so the people of Northwestern Ontario can receive quality care, closer to home.
Within Comprehensive Clinical Care, we have identified the following Goals:
- Adopt the Ontario Chronic Disease Prevention and Management framework;
- Deliver comprehensive cardiovascular care in accordance with the Ministry of Health;
- Enhance access to clinical services supported by patient flow efficiencies;
- Develop formal partnerships to deliver comprehensive clinical services that support care in the appropriate location;
- Deliver a comprehensive acute pain management service.
We will know we are successful by 2020 when we demonstrate:
- Patients with chronic illness possess self-management skills;
- Access to comprehensive cardiovascular care service in NWO;
- Patient access, length of stay, admission and discharge process improved;
- Partnerships support care closer to home;
- Access to comprehensive acute & chronic pain management.
Learn more about our exciting progress in this area:
Perfusionists in Training: A Step Towards Implementing Cardiac Surgery
In preparation for the much anticipated implementation of cardiac surgery at our Hospital, two highly skilled staff members were sponsored to train as clinical cardiovascular perfusionists at the Michener Institute in Toronto.
Vascular Surgery and EVAR Advance Cardiovascular Care
The implementation of vascular surgery and on-site endovascular aneurysm repair (EVAR) now available in at our Hospital is a major milestone in the establishment of a full cardiovascular surgery program for Northwestern Ontario.
Regional Orthopaedic Program Enhances Patient Outcomes
A new program helps maximize health outcomes for patients with musculoskeletal disease and disability across the region, shifting musculoskeletal care into a truly integrated system of quality care, closer to home.
Adopting Ontario's Chronic Disease Prevention and Management Framework
The Health Sciences Centre is committed to improving the way we prevent and manage chronic diseases in order to improve quality of life for our patients. To help guide us, we’ve adopted elements of Ontario’s Chronic Disease Prevention and Management Framework.
Digital Order Sets Improve Patient Care
Order sets ensure everyone involved in the care team is informed and follows the same instructions. Thunder Bay Regional Health Sciences Centre is introducing a new way to implement order sets that will improve patient care.
Perfusionists in Training: A Step Towards Implementing Cardiac Surgery
In preparation for the much anticipated implementation of cardiac surgery at the Health Sciences Centre, two highly skilled staff members were sponsored to train as clinical cardiovascular perfusionists at the Michener Institute in Toronto.
The perfusionist is trained and educated as a member of an open-heart surgical team. They are responsible for the selection, setup, and operation of a mechanical device commonly referred to as the heart-lung machine. During many types of open-heart and thoracic surgery, the patient's heart is stopped and blood is diverted away from the heart and lungs. In effect, the heart-lung machine, and the perfusionist running it, does the pumping and breathing for the patient.
"The role of the perfusionist is very important. Without them, cardiac surgery as it exists today would not be possible," said Arlene Thomson, Director of the Health Sciences Centre’s Cardiovascular and Stroke program. "It’s exciting that two people from our team are training for this profession, especially since perfusionists are in short supply across North America. It means we are one step closer to implementing the cardiac surgery program here at our Health Sciences Centre."
For Alexandra Brazeau, a Respiratory Therapist, the opportunity to become a perfusionist was just too good to pass up. She was aware of the perfusion profession but knew that without a cardiac surgery program at our Hospital it wasn't a viable option for her – until now. "I'm so thrilled that our Hospital chose to train current employees as opposed to recruiting an external perfusionist," she said. "I really look forward to completing my training and being a part of the cardiovascular surgery team."
Scott Longridge, RN and Emergency Department Coordinator also jumped at the opportunity to train as a perfusionist. "I find it very rewarding to be at the ground level of establishing such an important new program in our community," he said. "With our aging population and the high incidences of cardiac disease in Northwestern Ontario, providing cardiac surgery here is becoming more and more crucial. It will be a huge benefit to our patients and families, and I'm happy to be a part of it."
Alexandra and Scott are currently participating in the intensive, 19 month Michener Institute program, which is accredited by the Canadian Medical Association. Upon graduation, they will be eligible to write the certification exams of the Canadian Society of Clinical Perfusion and the American Board of Cardiovascular Perfusion.
To learn more about cardiovascular care at our Health Sciences Centre, visit www.tbhrsc.net.

Alexandra Brazeau and Scott Longridge are two dedicated Health Sciences Centre employees who temporarily relocated to Toronto to train as clinical cardiovascular perfusionists, which are crucial members of an open-heart surgical team.
Vascular Surgery and EVAR Advance Cardiovascular Care
The implementation of vascular surgery and on-site endovascular aneurysm repair (EVAR) now available in at Thunder Bay Regional Health Sciences Centre is a major milestone in the establishment of a full cardiovascular surgery program for Northwestern Ontario.
The Honourable Dr. Eric Hoskins, Minister of Health and Long-Term Care, and the Honourable Bill Mauro, MPP, made a special visit to our Hospital to help celebrate the exciting advancement in comprehensive cardiovascular care.
EVAR is a minimally invasive surgery in which a modular stent graph is inserted into the femoral artery and passed up into the weakened part of the aorta. Prior to this development, patients requiring this potentially life-saving procedure had to travel outside of the region to access the service.
David Stephens was the first patient to undergo EVAR at our Hospital in January 2017, and knows first-hand how important it is to have access to cardiovascular care in our region. “Learning that I could receive my treatment here at Thunder Bay Regional Health Sciences Centre was a huge relief,” he said. “Undergoing a medical procedure is stressful enough without the added difficulties of having to travel and leave your support team behind. I am so thankful for the excellent quality of care that I received right here at home.”
"Admission rates for cardiovascular patients at our Hospital are well above the provincial average. Our patients and their families deserve local access to care," said Grant Walsh, 1st Vice Chair, Thunder Bay Regional Health Sciences Centre Board of Directors. "This recent accomplishment reflects our commitment to meet the needs of our region through improved access to cardiovascular care, which will dramatically improve the quality of care and quality of life for thousands of patients."
This accomplishment stems from a partnership with the University Health Network (UHN), which began in 2015. The partnership has and will continue to be instrumental in Thunder Bay Regional Health Sciences Centre’s quest to expand and improve our comprehensive cardiovascular care program in accordance with the Ministry of Health and Long-Term Care, ensuring access to the highest quality of care, close to home.
"This is an important step forward for our Hospital and we couldn't have done it without our valuable partners at the University Health Network," said Jean Bartkowiak, Hospital President and CEO, and CEO of Thunder Bay Regional Health Research Institute. "We are committed to meeting the specialized acute care needs of the people of Northwestern Ontario. The arrival of vascular surgery and the ability to provide potentially life-saving procedures such as EVAR brings us one step closer to where we should be in terms of providing comprehensive cardiovascular surgery, closer to home."

From left to right: David Stephens, first EVAR patient at Thunder Bay Regional Health Sciences Centre, Honourable Bill Mauro, MPP, Jean Bartkowiak, President and CEO of Thunder Bay Regional Health Sciences Centre, Honourable Dr. Eric Hoskins, Minister of Health and Long-Term Care, and Dr. Mark Henderson, Executive Vice President of Patient Services at Thunder Bay Regional Health Sciences Centre.
Regional Orthopaedic Program Enhances Patient Outcomes
A new program helps maximize health outcomes for patients with musculoskeletal disease and disability across the region. The North West LHIN Regional Orthopaedic Program, launched in April 2016, shifts musculoskeletal care into a truly integrated system of quality care, closer to home.
While the Regional Orthopaedic Program is still new, Caroline Fanti, Regional Orthopaedic Program Director, is confident in its potential to grow and improve. "This program has already transformed the way we approach musculoskeletal care in Northwestern Ontario. We're also taking on a more holistic approach to care, so non-surgical patients will benefit as well. By working together, we can make a positive impact at a systems level and provide exceptional patient care that is sustainable."
"Residents of Northwestern Ontario face a higher than average prevalence of musculoskeletal disease and require higher than average use of orthopaedic surgical services in the region," said Fanti. "Under our new program, care is designed and delivered to address the health care needs and preferences of our patients and families across the region in order to be both appropriate and cost effective while maximizing health outcomes and the overall patient experience."
The Health Sciences Centre worked in partnership with the NW LHIN, as well as Dryden Regional Health Care, Riverside Health Care in Fort Frances, and Lake of the Woods District Hospital in Kenora. One of the main goals of the program is improved access and a standardized level of care for patients throughout the region.
"The program will provide appropriate, timely and equitable access to orthopaedic specialist care for patients and primary care providers through a user-friendly, centralized referral intake process and a regionally coordinated assessment mechanism," said Dr. David Puskas, Regional Medical Director of Musculoskeletal Health. "Care providers can now deliver a seamless experience of care so that our patients receive the right care, at the right place, at the right time."
"Process evaluation is also being undertaken in order to optimize wait times for emergent and non-emergent surgical cases for local and regional patients," said Adam Vinet, Director of Surgery.Quality and safety will be improved under the new program through the consistent implementation of evidence based best practices across the continuum of care. "Patients benefit from regional integration because it decreases variances in care through standardization, improved coordination, and transitions throughout the system," explained Dr. Rhonda Crocker Ellacott, EVP, Patient Services, & Chief Nursing Executive.

The Regional Orthopaedic Program has transformed the way we approach musculoskeletal care in Northwestern Ontario. (From left to right: Dr. David Puskas, Regional Medical Director of Musculoskeletal Health, Caroline Fanti, Regional Orthopaedic Program Director, Dr. Rhonda Crocker Ellacott, EVP, Patient Services, & Chief Nursing Executive, and Adam Vinet, Director of Surgery)
Adopting Ontario's Chronic Disease Prevention and Management Framework
Chronic diseases are the most common and costly health problems facing Canadians. As part of our commitment to delivering comprehensive clinical care, Thunder Bay Regional Health Sciences Centre has made chronic disease prevention and management a priority.
"Chronic diseases are long-term ailments that develop slowly over time that can often be prevented or controlled, but rarely cured. Diabetes, cardiovascular diseases, chronic respiratory diseases and cancer, along with mood and anxiety disorders, account for about one third of direct health care expenditures in Canada," explains Aaron Skillen, Program Director, Chronic Disease Prevention and Management. "We’re committed to improving the way we prevent and manage chronic diseases in order to improve quality of life for our patients. To help guide us, we’ve adopted elements of Ontario’s Chronic Disease Prevention and Management Framework."
Ontario’s Framework has eight elements that our Hospital will adopt:
- Health Care Organizations
- Personal Skills & Self Management Supports
- Deliver System Design
- Provider Decision Support
- Information Systems
- Healthy Public Policy
- Supportive Environments
- Community Action
To ensure that chronic disease prevention and management remains a focused priority, the Hospital has created a Steering Committee to oversee the development, implementation, and success of the framework. It also serves to bring together experts from all areas of the hospital to contribute to the development and implementation of new initiatives.
"Our Chronic Disease Prevention and Management Steering Committee engaged with internal and external partners in care and used the gathered feedback to develop one or two initiatives for each element of the framework," said Skillen. "For example, we plan to develop a chronic disease self management portal which will allow staff to provide more information to their patients on discharge as it relates to self management, helping patients to be more independent and self-sufficient in their care."
Effective chronic disease management includes the implementation of prevention measures to halt the disease's progress and to prevent complications. Initiatives at the Hospital include the Healthy Workplace, Smoke Free Together and Eating Healthy Together models.
"While still in the early planning stages, these initiatives combined should improve our Hospital's chronic care delivery system and help us to provide more effective care and better health outcomes," said Skillen. "And, as always, our Patient and Family Centred Care philosophy will ensure that our patients and families remain equal partners in their own health and full collaborators in managing their chronic conditions."
Moving forward, the Chronic Disease Prevention and Management Steering Committee will meet quarterly to review the action plan and discuss any barriers, solutions and successes. Once finalized, the plan will be in place for the next three years, helping to ensure we remain Healthy Together.

To ensure that chronic disease prevention and management remains a focused priority, the Hospital has created a Steering Committee to oversee the development, implementation, and success of Ontario’s Chronic Disease Prevention and Management Framework.
Digital Order Sets Improve Patient Care
When you are admitted to hospital, the next steps in your health care journey are identified and recorded. This system, called order sets, ensures everyone involved in your care team is informed and follows the same instructions. Thunder Bay Regional Health Sciences Centre is introducing a new way to implement order sets that will improve patient care.
Following a patient diagnosis, order sets are approved and assigned by a physician. They are used by clinicians and guide standard procedures and patient care plans from admission to discharge and include steps for care such as the types of medical tests and diagnostics required, or medications to be prescribed. Order sets are research based and standardized to support high quality, safe health care.
Traditionally, order sets are printed out on paper and hand-signed by the primary physician. To improve the process, our Hospital is saying farewell to paper and adopting digital order sets. This improves patient care and is part of the Hospital’s commitment to adopt standardized processes, tools, templates and resources that support quality care.
"Transitioning to digital and customizable order sets will support patient-centred care and promote a culture of quality and safety," said Dr. Gordon Porter, Thunder Bay Regional Health Sciences Centre Chief of Staff. "Digital order sets find the right balance between efficiency and accessibility. Physicians having increased and convenient access to standardized, evidence based will help improve patient safety."
The adoption and implementation of the digital, quality based procedure order sets was sponsored by the Ministry of Health and Long-Term Care. Think Research will oversee the provincial effort to digitalize the current paper based QBP Order Set inventory that is specific to our Hospital.
Using a standardized, digital approach to order sets is a significant process improvement that supports the quality improvement initiatives and enhances outcomes for patients. "Standardizing practice through common order sets reduces clinical variability and allows for quality patient care ordered in a consistent and reliable manner," said Porter. "Access to evidence-based guidelines at the bedside supports clinical decision making and reduces the potential duplication of medical orders. Going digital also enables real-time data analytics that can help inform and guide continuous quality improvement in key areas of cost, readmissions, safety and length of stay."

Dr. Gordon Porter, Chief of Staff at Thunder Bay Regional Health Sciences Centre, believes that transitioning to digital and customizable order sets will support patient-centred care and promote a culture of quality and safety.
Seniors' Health
The population of seniors is growing. Baby boomers' health care needs will continue to increase. We recognize that the care needs of seniors are different, and will tailor services to accommodate them.
To advance care for the aging population, we will focus on these Goals within Seniors' Health:
- Deliver an optimal experience for seniors;
- Adopt the Ontario Senior Friendly Hospital Framework.
We will know we are successful by 2020 when we demonstrate:
- Seniors' hospital experience is optimal;
- Seniors and their families are highly satisfied and engaged in care.
We have made progress in this area already. These stories are examples of initiatives that are underway.
Nurses Leading the Way to a More Senior-Friendly Environment
Some of our nurses have completed NICHE, a special nurse-driven training program to help improve the care we provided to senior patients.
Preventing Pressure Ulcers to Optimize Seniors' Care
Seniors are at an increased risk of pressure injuries because of changes to the skin that are part of the normal aging process. Preventing pressure injuries from occurring is one of the ways our Hospital can deliver an optimal experience for seniors.
Clinical Pathways Support Frail Seniors' Care in the Emergency
A new program has been introduced that begins in the Emergency Department (ED) at the Thunder Bay Regional Health Sciences Centre to speed up the assessment process of frail seniors, while ensuring that they receive the care and services they need.
Nurses Leading the Way to a More Senior-Friendly Environment
The population of seniors is growing in Northwestern Ontario. At Thunder Bay Regional Health Sciences Centre, we recognize that the care needs of seniors are different and we are committed to tailoring our services to accommodate them. A targeted group of Nurses have completed NICHE training, which is a special nurse-driven training program to help improve the care we provide to senior patients.
NICHE (Nurses Improving Care for Health System Elders) is the leading nurse-driven program that provides principles and tools to stimulate changes in culture of health care facilities to support patient and family centred care for older adults.
"The world's population is aging. Every day, 10,000 baby boomers turn 65, so it's crucial that health care providers prioritize the unique needs of the population," said George Fieber, Nursing Practice Leader. "That is why our Hospital, along with over 600 others across North America, Australia and Singapore, are partnering in NICHE to improve the care and services that we provide to patients age 65 and older."
In support of our coaching and learning, four members of our Nursing Leadership Team have recently completed the intensive six-week NICHE Leadership Training Program. This leadership program links internationally recognized clinical nursing experts in the field of acute care and geriatrics to our hospital to provide mentorship and support. Since graduating, our nurses have begun developing protocols and innovations in nursing practice that will help to enhance the patient and family experience.
"Nursing practice innovations will be launched over the next 12 months that focus on falls prevention, assessment and prevention of skin injuries, and reducing the incidence of urinary tract infections," said Fieber. "All of these interventions will contribute to creating a safer and more senior-friendly care environment at our Hospital." A number of nurses have completed a 22 hour on-line Geriatric Resource Nurse (GRN) course to help improve the care we provide to senior patients.
To learn more about how we’re prioritizing the care needs of seniors, visit www.tbrhsc.net.

Dawna Maria Perry, Director of Nursing; George Fieber, Nursing Practice Leader; and Bev Gellert, Nurse Manager 2A Medical, are three members of our nursing leadership team who have recently completed the Nurses Improving Care for Health System Elders (NICHE) training.
Preventing Pressure Ulcers to Optimize Seniors' Care
Pressure injuries (also called bedsores or pressure ulcers) are injuries to skin and tissue caused by prolonged pressure. Preventing pressure injuries from occurring is one of the goals set by Thunder Bay Regional Health Sciences Centre in order to deliver an optimal experience for seniors.
Pressure injuries most often develop on skin that covers the bony areas of the body, such as the hips, ankles, heels and the tailbone. Hospital patients and people who have a medical condition that limits their ability to change position, such as those confined to a wheelchair or bed, are at risk for developing pressure injuries.
Seniors are at an increased risk of pressure injuries because of changes to the skin that are part of the normal aging process. Pressure injuries can lead to serious infections, or further complicate existing medical conditions, resulting in longer hospital stays and delays in returning home.
"At our Hospital, we've made seniors' health a priority. We strive to provide an environment that minimizes the vulnerability of senior patients and promotes safety, comfort, independence, and functional well-being," said George Fieber, Nursing Practice Lead. "That’s why we are so diligent about pressure injuries - regular assessments and early intervention to prevent these types of injuries is one way we provide quality care."
Our nurses use an evidence based assessment tool called the "Braden Skin Risk Assessment" to identify those patients who might be at risk for developing a pressure injury. Patients with limited physical mobility are assisted with repositioning and with hygienic care. Patients assessed as being at high risk may also be referred to other members of our interprofessional team including specialist physicians, physiotherapists, occupational therapists, clinical dieticians and our clinical nurse specialist for wounds.
Tips to reduce your chances of developing a pressure injury in the community or hospital include:
- Change your position at least every two hours when you are in bed
- Change your position as often as possible while sitting
- Lift your body instead of dragging it when you are moving or changing position
- Keep the head of your bed as low as you can tolerate when you are sleeping to prevent sliding motion
- If your skin is being exposed to bodily fluids (sweat, urine, stool) more often, tell your caregiver or hospital staff
- Check your skin when you go to bed and before you get out of bed in the mornings
- Keep your skin clean and dry
- Check with your health care team to see if using a moisturizer (cream) would help
- Drink lots of fluids and eat a well-balanced diet
To learn more about how the Hospital has prioritized Seniors’ health, visit www.tbh.net.

Senior patients with limited physical mobility are at an increased risk of pressure injuries. One of the ways we provide quality care to our senior patients is by ensuring regular assessments and early intervention (such as assistance with repositioning and hygienic care) to help prevent pressure injuries from occurring.
Clinical Pathways Support Frail Seniors' Care in the Emergency
A new program has been introduced that begins in the Emergency Department (ED) at the Thunder Bay Regional Health Sciences Centre to speed up the assessment process of frail seniors, while ensuring that they receive the care and services they need.
Through collaboration with internal and external partners, consultation with geriatricians, ED physicians, St. Joseph’s Care Group, and the North West Community Care Access Centres (CCAC), the Frail Senior’s Pathway was developed to streamline access to care for the elderly.
"We recognize that when a frail senior patient presents in the Emergency Department, one of three things usually occurs: they have an acute illness that requires immediate admission to hospital; they have a condition that can be addressed in an inpatient rehabilitative setting; or they can be discharged home with necessary outpatient supports or services in place," said Ron Turner, Senior Director of Patient Services. "With the help of funding from the NW LHIN, our group came together to create a process and a standardized assessment tool that would help determine our patients' needs more effectively."
Getting patients the right care at the right time is always important, and especially crucial in the case of our frail senior population. Turner said that by assessing patients earlier and making informed decisions about their care, they hope to avoid unnecessary admissions to hospital. Research has shown that prolonged hospital stays can lead to further complications, particularly for this patient group.
"An elderly person who is admitted to hospital can deteriorate alot faster than a younger patient. Without comprehensive rehabilitative services, there is the potential for our frail seniors to lose up to 5% of their functional ability per day while in hospital. As a result, discharge to home may no longer be possible, and an alternate level of care would be required."
The new clinical pathway is supported by a Geriatric Care Coordinator. This nurse begins the patient assessment as quickly as possible and works with physicians and other clinicians to support the admission of patients, make referrals, and arrange transfers of care as needed. The Geriatric Care Coordinator coordinates with health care providers to ensure that services are in place before the patient is discharged from the Hospital.
"Having someone on the team who is directly responsible for organizing the care needs for these patients helps build confidence in the new process, and ensures that patients will get the appropriate level of care they need," Turner said.
The standardized assessment has also strengthened the relationship with health care system partners. "With the standardized assessment, our community partners are confident that patients are being referred to them based on the type of care or services they provide."
Program planning began in January 2017, and the clinical pathways have been trialed in the ED. Turner said that it’s still early, but so far results are promising.
"It's really about having a collaborative approach to ensure that patients are assessed early and that the appropriate patient care can be coordinated and provided as quickly as possible."

The Frail Seniors Clinical Pathway will help assess geriatric patients in the Emergency Department faster to ensure they are getting the level of care they need and to avoid unnecessary hospital admissions.
Indigenous Health
Enhance culturally appropriate care.
Indigenous people, particularly those from remote communities, face unique challenges to access to health care. In addition to geographical, language and cultural barriers, there are socioeconomic realities that simply do not exist outside of this population. Indigenous people account for at least 19% of our population. Unfortunately, they are the least healthy people in our region.
We aim to improve experiences and outcomes for Indigenous patients and families by providing care that is culturally relevant and sensitive, in welcoming environment.
Our Indigenous Health Goals are:
- Provide care that improves self-management, access, experience, and transition to home for Indigenous patients;
- Provide health care that respects traditional knowledge and practices, and builds TBRHSC as a leader in the provision of health care for Indigenous patients.
We will know we are successful by 2020 when we demonstrate:
- Indigenous patients from remote communities equally access, self-manage and transition to home;
- Indigenous people feel welcomed.
Please read about recent activities in this area.
Discharge Planning Eases Transition to Home for Indigenous Patients
The development of a discharge planning group is part of the Hospital’s commitment to provide care that improves self-management, access, experience and transition to home for Indigenous patients.
Supporting Indigenous Communities to Get Screened
Our Hospital has taken a new, more inclusive approach in order to help improve access to potentially life-saving cancer screening services for Indigenous communities.
Ojibwe Lessons to Foster a More Welcoming Environment
Our Hospital offers Ojibwe lessons to staff and volunteers. It's part of a commitment to enhance a welcoming environment for Indigenous patients and families.
Discharge Planning Eases Transition to Home for Indigenous Patients
Discharge plans support patients to transition from hospital to home. They include the steps to be taken and the services that need to be in place to ensure a safe transition to home. A discharge plan must be in place before an admitted patient is released from Thunder Bay Regional Health Sciences Centre. This process is different, and often more difficult, for patients returning to remote, northern communities. A new discharge planning group is working to help ease the transition to home for Indigenous patients and families.
The discharge planning group is part of our Hospital’s commitment to provide care that improves self-management, access, experience and transition to home for Indigenous patients. It also helps ensure coordinated follow-up care prior to discharge for patients from remote communities.
"Discharging patients to remote communities is a very complex process with specific considerations, such as Non-insured Health Benefits approvals, funding, geographical and travel limitations, and availability of services in the community," said Samantha Moir, Manager of Corporate Patient Flow. "The goal of the discharge planning group is to provide the necessary information and resources to health care providers who are involved in discharge planning to make the process as smooth and standardized as possible."
Our Hospital believes in the power of partnerships. The discharge planning group consists of numerous community partners, all working together to achieve a common goal - to enhance patients’ experiences and outcomes, while helping them to avoid waiting in the hospital any longer than necessary.
The group includes representatives from different departments within our Hospital, the Regional Palliative Care Program, Dilico Anishinabek Family Health, Nishnawbe Aski Nation, Non-Insured Health Benefits, and Wequedong Lodge. Everyone shares their expertise of the special considerations for discharging Indigenous patients to remote communities.
"So far, our focus has been on the development of resources to assist staff to best meet the needs of Indigenous people during their hospital stay and through to discharge to their remote communities," said Moir. "By making key information available to staff, we are improving discharge planning processes, decreasing length of stay, and improving communication and understanding between our Hospital and community health providers."
"We need to work together in order to make these transitions easier for both the patient and health care provider," said Susan Bale, member of the Discharge Planning Group. "Having a verbal dialogue between our Hospital and community care teams are essential in this process".

The Health Sciences Centre’s discharge planning group includes representatives from different departments within the Hospital, the Regional Palliative Care Program, Dilico Anishinabek Family Health, Nishnawbe Aski Nation, Non-Insured Health Benefits, and Wequedong Lodge. Together, they help to ease the transition to home for Indigenous patients and families.
Supporting Indigenous Communities to Get Screened
Cancer screening is the key to detecting cancer early, when it is the most treatable. Unfortunately, accessing screening services can be far more challenging for those living in remote, Northern communities. Thunder Bay Regional Health Sciences Centre has taken a new, more inclusive approach in order to help improve access to potentially life-saving cancer screening services for Indigenous communities.
"Screening leads to early detection of cancer, which will often be the difference between recovering from or dying of cancer," said Cathy Paroschy Harris, Director of Prevention and Screening Services. "Everyone should have access to cancer screening and have the opportunity to fully understand its importance. We need to do as much as we can to ensure access to screening in our geographically challenging area is as equitable as possible."
Prevention and Screening Services promotes and educates the public and primary care providers about cancer prevention and cancer screening in Northwestern Ontario. They also provide cancer screening services to adults who are eligible to be screened, through provincial screening programs using innovative approaches to technology like the Screen for Life Coach.
The Coach provides patients with access to three organized cancer screening programs; breast, cervical, and colorectal. It travels across Northwestern Ontario – including remote Indigenous communities - where the geographic distance from hospitals has typically kept rates of these potentially life-saving screenings down. Where colorectal and cervical cancer screening is available across Northwestern Ontario, the Coach is the only mobile mammography screening service to Indigenous communities. Prevention and Screening Services continues to embrace and grow the practice of empowering Indigenous communities to get more involved and help increase the number of people taking advantage of screening services.
"Our community driven approach to screening and education involves working closely with Indigenous communities to earn their trust and learn from them about how they want to receive our services," said Tarja Heiskanen, Manager of Screening and Assessment Services. "It’s an ongoing process of identifying what has worked in the past and how we can build on those successes together. Essentially, the communities design how they want our services to run and how those services should be promoted. Our goal is to build on the strengths of each community and be as flexible and responsive as we can to address specific needs."
The community based approach relies on partnership and collaboration between Prevention and Screening Services and communities, and involves working closely with Indigenous health centres, chiefs, and the community members themselves. This has required a great deal of education and commitment from the Prevention and Screening Services team, who continue to undergo cultural competency, relationship building and sensitivity training in order to strengthen trust and communication.
The Prevention and Screening Service currently works with over 45 Indigenous communities across Northwestern Ontario. To learn more, please visit http://tbrhsc.net/programs-services/prevention-and-screening-services/screening/.

Tarja Heiskanen, Manager of Screening and Assessment Services, and the rest of the team currently works with over 45 Indigenous communities across Northwestern Ontario.
Ojibwe Lessons to Foster a More Welcoming Environment

Esther Diabo, certified Native Language instructor, provides cultural teachings as well as Ojibwe language lessons to Hospital staff and volunteers.
Boozhoo. Miigwech. A simple greeting. A few familiar words spoken in your own language. They can go a long way to make you feel more comfortable and at ease when you're away from home. That's why Thunder Bay Regional Health Sciences Centre offers Ojibwe lessons to staff and volunteers. It's part of a commitment to enhance a welcoming environment for Indigenous patients and families.
The lessons, delivered by certified Native Language instructor Esther Diabo, provide cultural teachings as well as Ojibwe language.
Georgia Carr, Manager, Laboratory Services, participated in the very first session of Ojibwe classes. "I learned some words to help me communicate better. It shows respect, acceptance and belonging," she said.
Diabo structures the classes for a health care environment. She aims to help Hospital staff and volunteers to be able to welcome patients and families, introduce themselves, and understand and communicate simple phrases. She also shares teachings through stories, crafts and activities. For example, class participants take part in smudging ceremonies and make their own Dream Catchers.
"I was especially moved by what I learned about residential schools and culture," Carr said. "Esther was so open about her life stories, and tied them to her culture. I gained such an understanding and appreciation for the historical struggles."
So far, 34 people have participated in the classes, which are voluntary and provided at no cost to participants. Our Hospital serves all of Northwestern Ontario, which is home to 69 First Nation communities, many of them remote and difficult to access. For many people from remote First Nation communities, a visit to our Hospital can be intimidating, often because of language barriers.
"This knowledge supports us to be more understanding, more welcoming. We are so fortunate that Esther is willing to share and teach," noted Carr.

Georgia Carr, Manager, Laboratory Services, participated in the very first session of Ojibwe classes and appreciates the knowledge that Esther passed on to her. The teachings support Hospital staff to be more understanding and welcoming to Indigenous patients and their families.
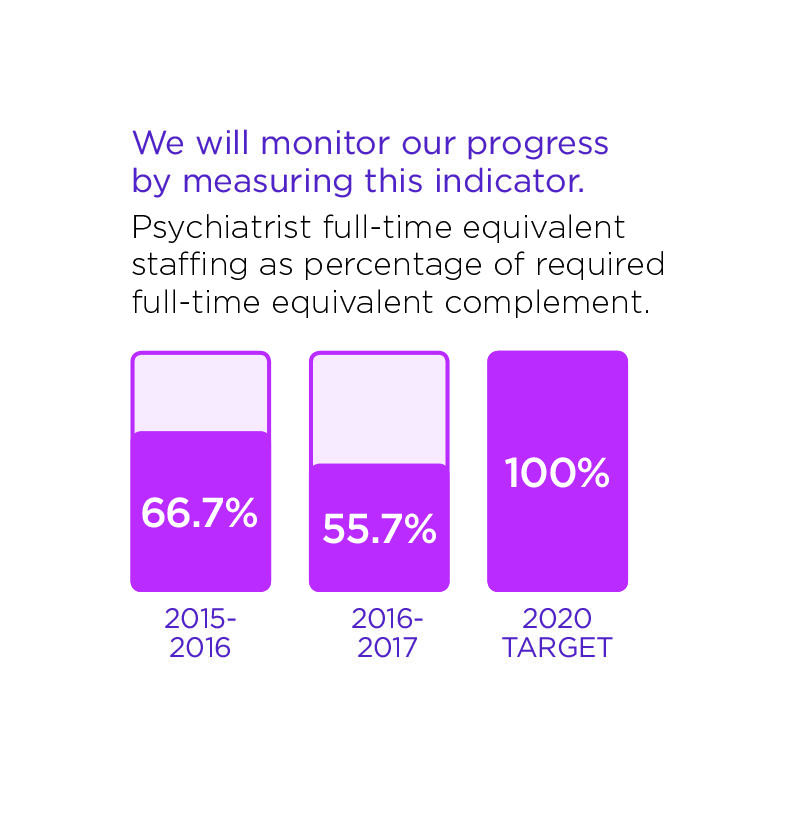
Acute Mental Health
Enhance acute mental health service.
While Acute Mental Health inpatient days are decreasing at other hospitals, it has increased by 5.4% here. We want to be sensitive to patient needs, ensuring that mental health is viewed as part of overall health. We believe that everyone should be respected equally, regardless of age, illness or culture and will strive to provide a more holistic approach to treat the full human being – mind, body, and soul.
Within Acute Mental Health, we will:
- Adopt attitudes and behaviours that recognize mental health as an integral part of the delivery of comprehensive acute care services;
- Enhance the delivery of mental health care to patients outside of mental health services;
- Collaborate with system partners and appropriate governing agencies to develop and enhance transition in care;
- Enhance the delivery of acute mental health care within mental health services.
We will know we are successful by 2020 when we demonstrate:
- The hospital supports a stigma-free environment;
- Access to Psychiatry service.
These stories provide examples of our commitment in action.
Providing Safer Care to Inpatients Struggling with Mental Health
The Adult Mental Health department has identified steps that can be taken to improve care and make the Hospital environment safer for mental health patients outside of the Acute Mental Health unit.
New Test Helps Identify Patients Struggling with Mental Health
A new screening tool at the Thunder Bay Regional Health Sciences Centre is designed to identify inpatients who may be struggling with mental health issues by asking four simple questions at admission.
Providing Safer Care to Inpatients Struggling with Mental Health
Mental health inpatient rooms look much different than your typical hospital room at the Thunder Bay Regional Health Sciences Centre. They are made safer for patients who may be at a higher risk of hurting themselves and others. For example, there are no long cords, clothes hooks are all break-away, and we minimize easy to move objects in the room.
However, some patients struggling with their mental health may also have physical health issues that need to be treated in the ICU, surgical recovery, or some other medical unit in the hospital.
"We have many mental health off-service patients who cannot be moved to the mental health unit until their medical conditions have been addressed," said Dr. Peter Voros, Director of Adult and Forensic Mental Health. "Nurses who are on those floors don’t usually have the same speciality training as a mental health nurse."
The Adult Mental Health department identified steps that can be taken to improve care and make the environment safer. Dr. Voros and his team have updated the existing standard of care to provide specific guidance for health care professionals, particularly nurses, caring for off-service patients.
"The new policy gives specific direction in terms of what to do to make a patient's room as safe as possible," Dr. Voros said.
A large part of the initiative is simply to help nurses and other health care providers think about potential hazards in the room and within the unit. These include pull cords and the other items mentioned above as well as sharp items brought in and out of the room during the course of patient care (such as scissors for changing a dressing). Another consideration is that those who may be at higher risk need close monitoring.
"We are outlining how to look at the room and care for the patient through the lens of the mental health nurse," he said.
Martina Nuttal, a new clinical nurse specialist (CNS) who started in the Adult and Forensic Mental Health department in May 2017, is developing an educational package for staff. It’s another way to support the staff, and in turn support the patients.
"We want to do everything we can to help keep patients and our staff safe," Dr. Voros said.

Martina Nuttal, who joined the Adult and Forensic Mental Health department in 2017, will help health care professionals on medical units look at potential hazards through the lens of a mental health nurse.
New Test Helps Identify Patients Struggling with Mental Health
A new screening tool at the Thunder Bay Regional Health Sciences Centre is designed to identify inpatients who may be struggling with mental health issues. The pilot project, tested in the 1A unit this past spring, screened patients at admission by asking four simple questions. The test was so successful that it will be rolled out to other units starting this fall.
"We wanted to complete a pilot in one unit first before bringing it to other units to make sure it was useful for identifying patients who may need help," said Dr. Peter Voros, Director of Adult and Forensic Mental Health.
When a patient is admitted to a unit, nurses routinely test vital signs and do what’s called a medical history to understand past health issues. Previously, there were some mental health questions asked during the medical history, but this new set of questions – call the Patient Health Questionnaire-4 (PHQ-4) – is designed to score patients using a point system from 0-6 in both anxiety and depression. Patients that score a 3 or higher in either category are flagged for the patient’s physician.
However, a high score doesn’t necessarily mean there is a major problem. "All a positive screen means is that someone needs to ask more questions," said Dr. Voros. The physician decides the next appropriate steps including talking with the patient to learn more, possibly referring back to a family physician for follow-up on discharge, or making a referral to a psychiatrist, if needed.
The real strength of the screening tool is that it takes something that can be subjective – assessing a person’s mental health – and makes it easier for any health professional to determine when a patient may need some mental health care. It helps ensure patients get the right care they need, when they need it.
"This screening tool is standardized and it’s supported by research that says within a general population, if you score 3 or higher, there’s a chance that you may be struggling," Dr. Voros said.
The results from the pilot project were in line with expectations, he said. Of the 39 patients screened, five scored positive for anxiety and depression. Two were already receiving treatment and two were able to get a referral to a psychiatrist as a result of this new screening tool. (The fifth had already been transferred to long-term care, though a note about the positive score was forwarded to the care facility.)
The new initiative came as a direct result of the Strategic Plan 2020, which highlights mental health as a key area of focus. One of the goals is to improve mental health assessment within the patient history, which this screening tool has demonstrated it can do.
Dr. Voros said that the screening tool will be added to the admission process in all units by fall 2017. Currently, other supports are also being put into place including recruiting more psychiatrists and creating a Consultation Liaison Service. This service will be coordinated by a mental health nurse who will be able to provide an intermediate level of care between referring physicians and psychiatrists to streamline the process even further and ensure that patients are getting the right level of care.
With all of these pieces in place, the result will be a more proactive approach to helping inpatients at the hospital get the help they need for any mental health issues they are experiencing.
"It’s an opportunity for us as health care practitioners to make sure we’re asking the right questions and identifying where there may be difficulties," Dr. Voros said.

A new screening tool tested at the Health Sciences Centre will help health care professionals identify inpatients who may be struggling with their mental health.
The Impact of Your Donations at the Thunder Bay Regional Health Sciences Centre
Overall in 2016, your donations were responsible for providing $3,213,364 in funding which was distributed throughout the Thunder Bay Regional Health Sciences Centre, with an additional $91,824 provided to several hospitals across Northwestern Ontario for programs operated by the Health Sciences Centre. These funds guaranteed the purchase of critical equipment to ensure we have quality care here at home.
Examples of funded equipment include: Ventilators, an Ultrasound Machine, a Large Bore C/T Scanner, a Transfusion Medicine Analyzer, Vital Signs Monitors and much more.
Your donations continue to have a tremendous impact at the Health Sciences Centre. From gifts made to celebrate special occasions, to memorial gifts, to gifts made through a Will, you have shared your enthusiasm for health care that is second-to-none, here at home. The Thunder Bay Regional Health Sciences Foundation exists to serve you, our donors, to ensure your passions and dreams come to life through your gifts made in support of the Health Sciences Centre.
A full listing of grants made possible thanks to donors like you is available at: healthsciencesfoundation.ca/impact
Financial Statements
Thunder Bay Regional Health Sciences Centre continues to manage health care resources effectively and responsibly, while providing quality acute health care for the residents of Northwestern Ontario.
Our Health Sciences Centre continues to face service and financial pressures as a result of many fiscal, demographic and health care system challenges. In 2016/17, we regularly operated in surge capacity, and this creates significant financial pressures.
Our budgeted deficit for 2016/17 was $6.9 million. In addition to measures we took internally, we received one-time funding from the North West Local Health Integration Network and the Ministry of Health and Long Term Care to address a majority of the deficit.
We continue to work closely with the Local Health Integration Network and other community partners to address the ongoing challenges.
| FINANCIAL STATEMENTS | |||||||
| March 31, (Amounts in $ thousands) | 2017 | 2016 | 2015 | 2014 | 2013 | 2012 | 2011 |
|---|---|---|---|---|---|---|---|
| Assets | |||||||
| Current assets | 29,125 | 30,459 | 31,259 | 33,113 | 33,452 | 29,822 | 28,779 |
| Non-current assets | 241,497 | 252,981 | 272,029 | 260,039 | 238,660 | 246,473 | 256,185 |
| Total Assets | 270,622 | 283,440 | 303,288 | 293,152 | 272,112 | 276,295 | 284,964 |
| Liabilities and Fund Balances | |||||||
| Current liabilities | 46,199 | 45,067 | 57,169 | 45,300 | 42,858 | 41,179 | 40,175 |
| Non-current liabilities | 219,330 | 234,449 | 240,113 | 236,634 | 218,603 | 227,040 | 233,508 |
| Total liabilities | 265,529 | 279,516 | 297,282 | 281,934 | 261,461 | 268,219 | 270,498 |
| Fund Balances | 5,093 | 3,924 | 6,006 | 11,218 | 10,651 | 8,076 | 11,281 |
| Total Liabilities and Fund Balances | 270,622 | 283,440 | 303,288 | 293,152 | 272,112 | 276,295 | 284,964 |
| STATEMENT OF OPERATIONS | |||||||
| For the year ended March 31,(Amounts in $ thousands) | 2017 | 2016 | 2015 | 2014 | 2013 | 2012 | 2011 |
|---|---|---|---|---|---|---|---|
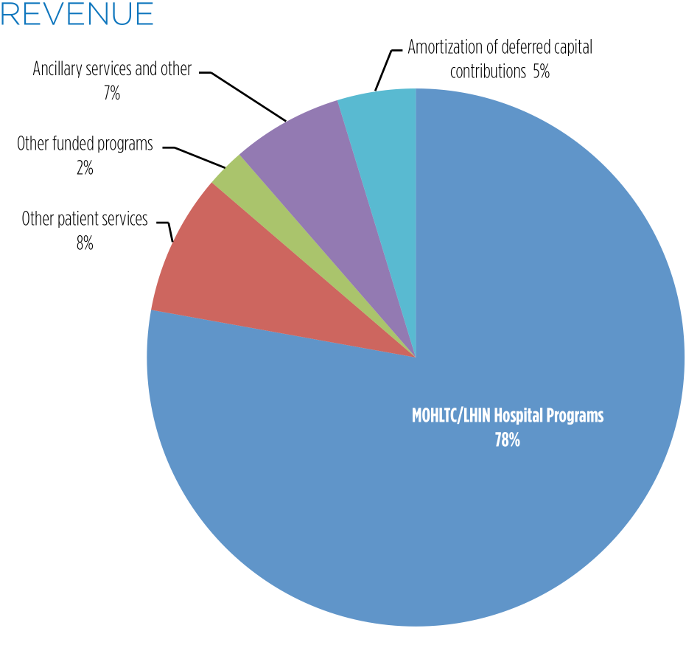
| Revenue | |||||||
| Ontario Ministry of Health and Long-Term Care/ North West Local Health Integration Network | 257,692 | 258,582 | 249,780 | 238,968 | 233,940 | 227,104 | 221,085 |
| Other patient services | 27,994 | 26,809 | 26,841 | 26,411 | 25,109 | 26,716 | 26,721 |
| Other funded programs | 7,693 | 11,593 | 10,863 | 9,671 | 8,838 | 8,727 | 7,312 |
| Ancillary services and other | 22,121 | 19,954 | 17,681 | 17,020 | 15,532 | 16,246 | 15,117 |
| Amortization of deferred capital contributions | 15,597 | 15,953 | 16,253 | 16,214 | 16,767 | 16,420 | 19,738 |
| 331,097 | 332,891 | 321,418 | 308,284 | 300,186 | 295,213 | 289,973 | |
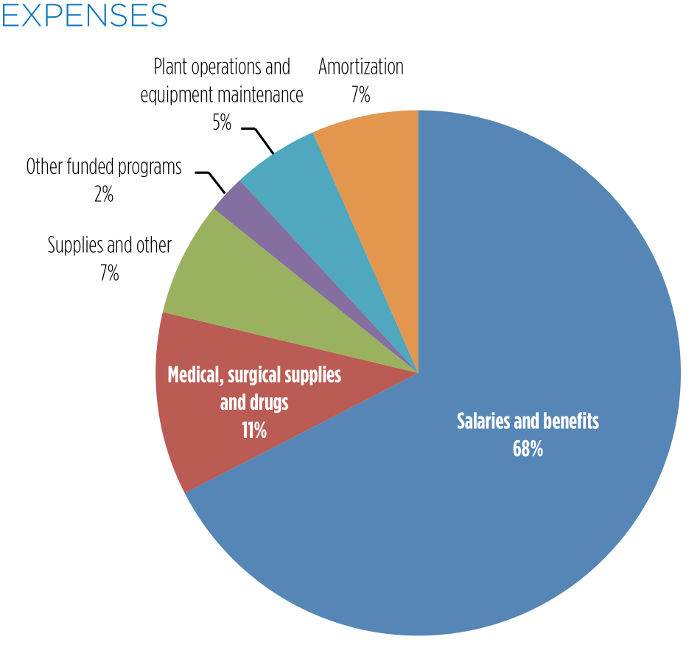
| Expenses | |||||||
| Salaries and benefits | 223,589 | 221,916 | 213,384 | 204,366 | 198,443 | 200,141 | 195,068 |
| Medical, surgical supplies and drugs | 37,409 | 38,315 | 40,059 | 36,064 | 34,486 | 34,919 | 33,866 |
| Supplies and other | 23,386 | 22,653 | 19,416 | 19,216 | 18,089 | 22,666 | 21,665 |
| Other funded programs | 7,702 | 11,764 | 10,981 | 9,647 | 8,840 | 8,744 | 7,226 |
| Plant operations and equipment maintenance | 17,643 | 17,687 | 17,665 | 16,252 | 15,874 | 10,517 | 13,614 |
| Amortization | 21,818 | 21,284 | 22,086 | 22,758 | 22,032 | 21,245 | 20,868 |
| 331,547 | 333,619 | 323,591 | 308,303 | 297,764 | 298,232 | 292,307 | |
| Excess (deficiency) of revenue over expenses | (450) | (728) | (2,173) | (19) | 2,422 | (3,019) | (2,334) |