Compre-
hensive
Clinical Care
Enhance the delivery of our clinical services.
Comprehensive Clinical CareThunder Bay Regional Health Sciences Centre
Our Vision
healthy
together
Our Mission
We will deliver a quality patient experience in an academic health care environment that is responsive to the needs of the population of Northwestern Ontario.
Our Philosophy
Patient and Family Centred Care is the philosophy that guides us. Patients and Families are at the centre of everything we do.
We will focus our efforts on Patient Experience, Seniors' Health, Comprehensive Clinical Care, Aboriginal Health and Acute Mental Health.
Our Values
Patients ARE First:
Patients and families at the centre of everything we do. At our world-class acute health care facility, we provide care to the people of Northwestern Ontario - a region the size of France with over 250,000 residents.
Ours is the teaching hospital of choice for over 1,500 learners from the Northern Ontario School of Medicine, Lakehead University, Confederation College, and other partnering academic institutions. We are an academic health sciences centre, committed to teaching the next generation of healthcare providers and advancing medical research. Patients benefit from interprofessional teams of healthcare providers and access to leading-edge medical equipment and clinical trials.
Providing effective health care for patients and families has earned us both Innovation Awards and Leading Practice Designations. We are a national leader in Patient and Family Centred Care.
The Health Sciences Centre belongs to the community it serves; the 250,000 residents of Northwestern Ontario. Our Strategic Plan 2020 was built by and for them.
We are pleased to provide this report on the 2015-2016 fiscal year progress of the Strategic Plan 2020.
Leader Messages
Message from the Chair of the Board of Directors

This past year, we said farewell to one President & CEO and welcomed a new one. We launched the Strategic Plan 2020, made progress towards developing a cardiovascular surgery program, and much more. While we embark on new and exciting times, I'm proud to say that one thing remains the same — our commitment to Patient and Family Centred Care (PFCC).
Our PFCC philosophy is the cornerstone of everything that we do, and it will continue to guide us as we accomplish the Directions set out in the Strategic Plan 2020. This plan was developed by our community members, for our community members. Over 1,300 people provided input into the plan and, as a result, their priorities are reflected in our five Strategic Directions: Patient Experience, Comprehensive Clinical Care, Seniors' Health, Indigenous Health and Acute Mental Health.
The Strategic Plan 2020 is a roadmap for our vision, to be Healthy Together. It provides the key milestones and criteria to our mission of delivering a quality patient experience in an academic health care environment that is responsive to the needs of the people of Northwestern Ontario. By keeping patients and their families at the centre of everything we do, we will surely achieve our goals.
Dr. Bill McCready, Interim President & CEO, was instrumental in the launch of the Strategic Plan 2020, and I speak on behalf of the Board of Directors as well as staff, physicians and volunteers in thanking him for his dedication and leadership. I'm also thrilled to welcome Jean Bartkowiak, who joined our team as the new President & CEO in January. He has an extensive background in hospital and health system leadership and I know he will help us achieve great successes moving forward.
As always, I am astounded at the dedication of our staff, physicians and volunteers in delivering on our mission and making our Strategic Directions a priority. They do this under challenging conditions – operating over capacity, caring for a population with the poorest health status in the province, in a remote geography – yet are unwavering in their commitment to delivering excellent specialized health care. I am humbled to serve as the Chair of an organization relying on such dedicated health professionals.
In closing, I emphasize that Thunder Bay Regional Health Sciences Centre is your Hospital and we are here to serve you in achieving our vision of Healthy Together.
Thank you.
Chair, Board of Directors
Message from the President and CEO

Although I wasn't here for the whole year, I can say with confidence that it has been a significant one for Thunder Bay Regional Health Sciences Centre.
Since my arrival, I have witnessed this organization's strong commitment to Patient and Family Centred Care. I am so proud to be part of a team that ensures the patients and their families are the focus of everything we do.
I also commend my predecessor, Dr. Bill McCready, under whose leadership the Strategic Plan 2020 was developed. The plan focuses on the directions that will be the most important and impactful for the community we serve. I am excited about the future of health care delivery in our region and look forward to accomplishing what the plan sets out to do.
There have already been successes. This past year saw formal provincial government support of our proposal to expand our cardiovascular services to provide a full range of cardiovascular surgeries at our Health sciences Centre, in partnership with the University Health Network (UHN). This new partnership will bring world-class cardiovascular care to Northwestern Ontario and have a dramatic effect on access to care ensuring improved care and quality of life for thousands of patients suffering from cardiovascular diseases in our region in the coming years. I encourage you to read about other areas of Strategic Plan 2020 progress.
While we implement our Strategic Plan 2020 to address the highest needs of patients and their families in Northwestern Ontario, we do so in an increasingly challenging health care system. The growing population of vulnerable patients with higher rates of chronic illnesses only further exacerbates what are already demanding fiscal pressures. We are still a young and growing academic health sciences centre, so it is important for us to work together with our system partners to ensure we accomplish our mission and priorities effectively and efficiently.
One of my main priorities is to address the Hospital's chronic overcapacity challenges. The key will be working with our health system partners and especially the primary care providers in Thunder Bay and surrounding areas to ensure we all fulfill our respective missions. This can be achieved. It has been done elsewhere and we will do it here.
Despite the ongoing challenges, it is an exciting environment with opportunities to innovate in health care delivery, teaching and research and to strengthen patient safety, quality, accountability and effectiveness for patients and their families.
Our successes to date are all thanks to the incredible efforts of all staff, physicians, volunteers, researchers and donors. This is an excellent organization. Together, we will make it even better.
Thank you.

President & CEO
Message from the Co-Chair, Patient and Family Advisory Council

What an exciting year it has been! As I reflect over the past year’s changes and successes, I realize that our Patient and Family Advisory Council at Thunder Bay Regional Health Science Centre has never been busier.
There is not a single area of our Hospital that doesn't have patients and families at the table contributing at all levels of decision making, both clinically and administratively. Having forged this partnership with patients and staff has had a tremendously positive effect on the overall patient experience. We know there is no other hospital that has its community more engaged than ours, and that is something to be proud of.
We are still the only hospital in Canada to hold Accreditation Canada's “Leading Practice” in Patient and Family Centred Care. We are also proud that this year we received two prestigious awards from the Canadian Patient Safety Institute (CPSI), one as an organization, and one for the work our Patient Family Advisors do. The CPSI is a national organization that monitors patient safety and patient experience across Canada.
As we enter this new fiscal year, I am excited to be doing so with a new President and CEO and a Strategic Plan that is all about meeting the specific specialized health care needs of the residents of our region. I have full confidence that by continuing to involve patients, their families and the community in all of our decisions, we will continue to achieve great successes.
Our past and future successes are because of great leadership, hard working staff, and an amazing group of volunteers. I am so very proud to be part of this award winning team that puts the PATIENTS and their families at the center of everything we do. I couldn't be more thankful for that.
Thank you.

Co-Chair, Patient and Family Advisory Council
Message from the Medical Advisory Committee

The Medical Advisory Committee has had a busy year working to ensure that Thunder Bay Regional Health Sciences Centre remains a leader in Patient and Family Centred Care. Everything we do is rooted in providing quality medical care, health education programs, health research, and patient safety.
This commitment is applied to all aspects of our role as a Medical Advisory Committee. This includes attracting, appointing and credentialing, as well as reappointing, all members of the Professional Staff, and ensuring that the Professional Staff responsibilities and accountabilities as defined in the By-Law, Hospital policies and Legislation are met. We are also responsible for assuring that quality medical care is delivered, that professional medical practice is monitored and advanced, and that Professional Staff function as partners in the care of patients.
I am proud of our commitment to support and provide learning opportunities for current and future health care providers. We've been able to accomplish this through mutually beneficial partnerships with the Northern Ontario School of Medicine, Lakehead University, Confederation College, and the Thunder Bay Regional Research Institute, as well as affiliations with approximately 50 other academic institutions around the world. As a relatively young academic health sciences centre, these partnerships are crucial. They help us to assess and align course curriculum and clinical experience with our academic partners, and provide us with the best and brightest new recruits.
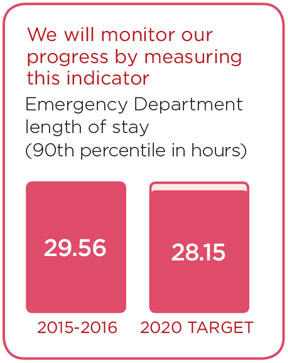
One factor that can impact our ability to deliver health care effectively and efficiently is length of stay – the amount of time a patient is admitted to our hospital. You’ve all probably heard of gridlock, and understand how it can negatively impact the patient experience. Reducing length of stays can maximize efficiencies and reduce hospital bed pressures, thereby reducing gridlock and improving the patient experience. This is an area where our Professional Staff was actively and successfully involved. We saw a slight reduction in our patients' length of stay and thankfully without any negative outcomes. We are poised to do even better in the coming years.
This is just the beginning of our journey to improve our provincial ranking of the expected length of stay performance, and we’ll continue working to reduce our average length of stay each year to meet the provincial expected length of stay target in 2020. We're currently working to identify barriers to timely discharge which will help direct our efforts towards unnecessary prolonged hospital stays. This has been, and will continue to be one of our main priorities.
Health care is a fast paced environment that is always evolving. It's important that we continue to grow as an academic health sciences centre and foster an environment of innovation and learning to advance a quality patient experience. By doing so, we will surely achieve our vision of being Healthy Together.
Thank you.
Acting Chief of Staff
Acting Chair, Medical Advisory Committee
Patient Experience
Enhance the quality of the patient experience.
We are leaders in Patient and Family Centred Care (PFCC), and it is the philosophy that guides us. We recognize that creating a quality patient experience builds upon this philosophy.
We are focused on enhancing the Patient Experience as one of our strategic priorities. Our goals are to:
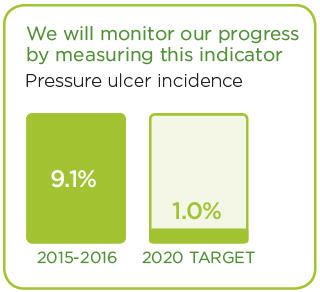
- Develop a framework to deliver high quality care;
- Enhance understanding and continue to grow and embed our PFCC philosophy;
- Advance the academic environment ;
- Invest in staff development, engagement and wellness;
- Use information technology to advance the patient experience.
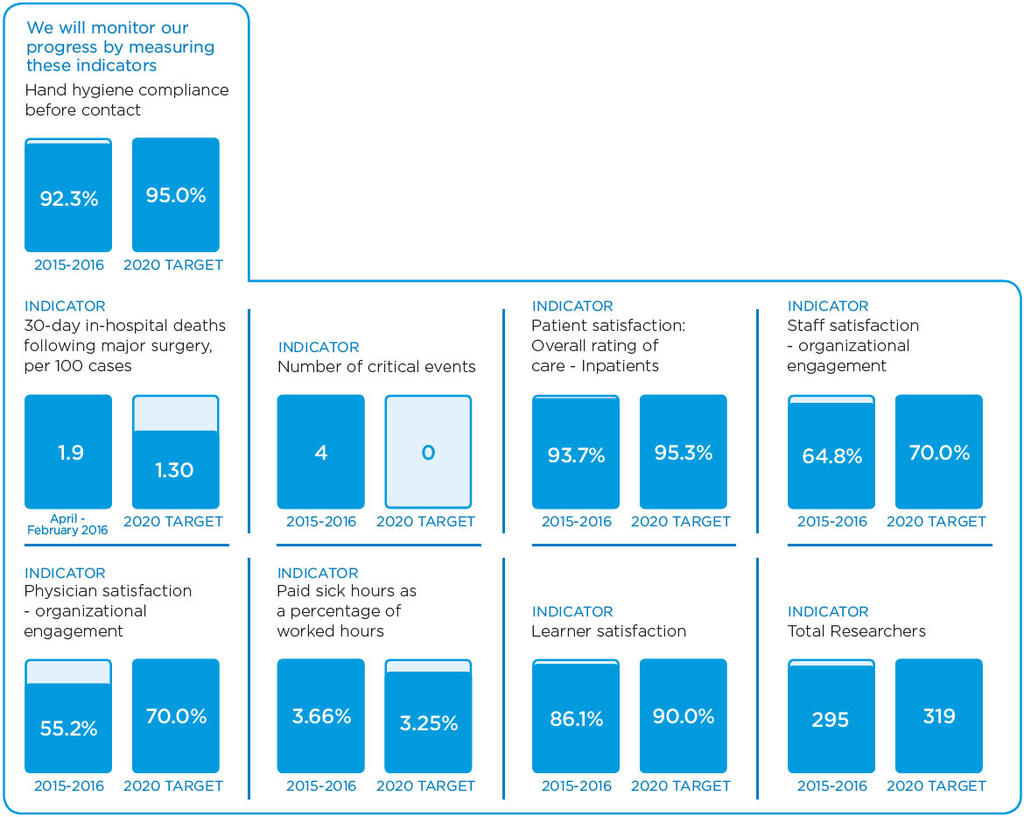
We will know we are successful by 2020 when we demonstrate:
- No harmful events;
- Patients are highly satisfied & engaged in care;
- A research culture;
- Learners are satisfied;
- Staff and physicians are engaged in care;
- Advanced information technology supports patients and care providers.
These stories provide an insight into two of the many Patient Experience initiatives in 2015/16:
Leading the Way to a Better Patient Experience
Great organizations stem from great leaders: We are investing in leadership to solidify our role as leaders in health care delivery.
Champions in Patient and Family Centred Care
Putting patients first: How “Physician Champions” value, support and promote PFCC.
Leading the Way to a Better Patient Experience
An organization must have great leaders. That’s why we are investing in leadership to enhance the overall quality of the patient experience.
Our Health Sciences Centre is already recognized as one of Canada’s 10 Most Admired Corporate Cultures. To build on that, we have engaged Studer Group Canada to implement a leadership enhancement training program that will help foster an even greater clinical, academic, and scientific environment for our patients and their families as well as our learners and researchers.
“It’s very exciting that our leadership team is embarking on this journey that will sustain and build upon the excellence that exists in our teams” said Amy Carr, Acting Senior Director, Human Resources. “Studer Group will offer a series of sessions to enhance our leaders’ staff engagement skills that will ultimately translate to an improved experience for our patients and families.”
Studer Group Canada is a health care consulting organization that supports other health care organizations in strengthening a sustainable corporate culture that promotes accountability, fosters innovation, and ensures consistent quality patient experience for better outcomes and satisfaction over time.
“We are committed to continuously improve care with more positive outcomes,” explained Carr. “We achieve that by fostering an unbreakable link between our corporate culture or values, our leaders’ engagement abilities, our staff behaviours, and the improvements we want to observe in the patient experience and the outcomes that are the bedrock of our mission, vision, values and strategic directions.”
We firmly believe that our commitment to excellence positively impacts not only patient and family satisfaction but also our performance while also engaging our staff and leaders to live our mission and values.
“As leaders in Patient and Family Centred Care, we know that providing a satisfactory patient experience is of utmost importance. We fully embrace this service improvement journey because it comes with a firm and measurable commitment to excellence,” said Jean Bartkowiak, President and CEO. “We want to make sure our employees feel valued, our physicians feel confident about the quality of care we are providing, and most importantly – that patients feel that the service and quality of care they receive here at our Health Sciences Centre are extraordinary.”
This process will further strengthen the already positive corporate culture that we are known for. It enhances an environment that naturally attracts and retains high performers and allows them to thrive, ensuring that we continue to flourish in the future.
“Our approach to leadership isn’t just about being a leader of people and employees, it’s also about solidifying us as a leader of health care delivery,” says Bartkowiak. “By combining proven best practices of leadership with leading edge clinical and relational practices, we will achieve greater successes in improving the overall patient experience.”

Trina Diner, Manager, Palliative Care and Telemedicine, TBRHSC, (right) “rounds” on Nancy Niemi, RN, TBRHSC, as part of the new leadership program. Staff rounding is a new way for management to meaningfully engage with staff on a regular basis.
Champions of Patient and Family Centred Care
Patient and Family Centred Care (PFCC) is the philosophy that guides us. A relatively new approach to health care, PFCC puts patients and families at the centre of everything we do and involves them in medical decisions like never before.
We’ve been practicing PFCC for the past six years, and the Strategic Plan 2020 displays our continued commitment to grow and embed the PFCC philosophy at our Health Sciences Centre.
"PFCC is not something that just happens," says Dr. Rhonda Crocker Ellacott, Executive Vice President, Patient Services and Chief Nursing Executive. "It’s about making an intentional commitment to a journey with a richer appreciation of what it means to work in collaborative partnership with patients and families. It changes the way you do business to shape a better organization.”
Our PFCC Leadership Council provides corporate leadership to advance Patient and Family Centred Care and ensures patient and families are at the centre of everything we do. The council is comprised of leadership representatives from all areas of the hospital, and works to create sustainable systems, structures and process for Patient and Family Centred Care. Two physicians also sit on the council to provide their valuable perspective. With such commitment and passion for PFCC, they have become “Physician Champions” of PFCC throughout the organization.
“In my opinion, PFCC has proven to be a major asset to our organization,” said Dr. Parvis Masoudi, PFCC Leadership Council Physician Champion. “As a physician, I feel PFCC has a positive impact on physicians' insight into our patients’ care. “As physicians, we really work together with the patient and their families. With their valuable feedback, we can adjust the care we provide based on their needs. It has done wonders to improve patient outcomes and satisfaction rates, and helps reduce length of stay. Enhancing patient-physician communication not only greatly benefits the patient; it has also improved physician satisfaction as well.”
“Although we are already recognized leaders in PFCC, we now view it as an ongoing commitment to better the overall experience of care,” said Dr. Crocker Ellacott. “It’s a journey, not a destination. As we continue on this journey, I am sure we will find more success for our organization, but most importantly, improvements that will be felt by our patients and their families.”

Patient and Family Centred Care is all about the collaborative partnership between patients, families and their care team. Above, Dr. Parvis Masoudi, PFCC Leadership Council Physician Champion, consults with a patient and his son to determine the best possible care plan.
Comprehensive Clinical Care
Enhance the delivery of our clinical services.
We aim to enhance the Comprehensive Clinical Care that transcends the organization and touches all patients. Our activities are focused on addressing gaps in care, so the people of Northwestern Ontario can receive quality care, closer to home.
Within Comprehensive Clinical Care, we have identified the following Goals:
- Adopt the Ontario Chronic Disease Prevention and Management framework;
- Deliver comprehensive cardiovascular care in accordance with the Ministry of Health;
- Enhance access to clinical services supported by patient flow efficiencies;
- Develop formal partnerships to deliver comprehensive clinical services that support care in the appropriate location;
- Deliver a comprehensive acute pain management service.
We will know we are successful by 2020 when we demonstrate:
- Patients with chronic illness possess self-management skills;
- Access to Comprehensive cardiovascular care service in NWO;
- Patient access, length of stay, admission and discharge process improved;
- Partnerships support care closer to home;
- Access to comprehensive acute & chronic pain management.
Learn more about our progress in this area:
New Vascular Services Already Producing Dramatic Results
People in Northwestern Ontario lose their limbs to amputation at a rate of 2.7 times greater than the provincial average: The arrival of cardiovascular services helps patients keep their limbs and their lives intact.
Easing the Pain: New Comprehensive Pain Management Program
Of all the symptoms patients experience while in hospital, pain may be the most distressing: New pain program deal with both acute and chronic pain for better patient outcomes.
New Vascular Services Already Producing Dramatic Results
People in Northwestern Ontario lose their limbs to amputation at a rate 2.7 times greater than the provincial average.
Many of these amputations would not have been necessary if the patient had received appropriate care sooner. The historic lack of cardiovascular services in this part of the province has contributed to the much higher loss of limbs found among patients here. A dramatic reverse of this inequity is coming.
Last June, the introduction of Comprehensive Cardiovascular Services at Thunder Bay Regional Health Sciences Centre was endorsed by the provincial government. The Program will save limbs for people in Northwestern Ontario.
It has already likely saved at least one.
Ms. Gaetanne Roy of Nakina feels lucky to still have all her limbs. She was the recipient of one of the first bilateral aortoiliac kissing stent insertion procedures performed at our hospital. The procedure was done by vascular surgeon Dr. Yaasin Abdulrehman and vascular interventional radiologist Dr. Anatoly Shuster. The two specialists were recruited to Thunder Bay as part of its first steps towards a cardiovascular service.
For Ms. Roy, the benefit cannot be overstated.
“Thunder Bay saved my leg,” she stated unequivocally.
Ms. Roy’s was a complicated case. She is diabetic and has a transplanted kidney. She was suffering from severe vascular disease, resulting in dramatic narrowing and blocking of arteries pumping blood to her legs and feet. She had developed ulcers on her foot. Her nephrologist Dr. Paul Watson, concerned she was in danger of losing her limb, referred her to Dr. Abdulrehman.
She was indeed. With the tissue loss from her condition, Roy had a 40 per cent chance of losing her leg within six months if her circulation wasn’t improved, said Dr. Abdulrehman.
“She certainly was high risk,” he said.
Previously, there would have been delays in getting her transported to Winnipeg or Toronto where she would see a vascular specialist. Those delays would have increased the likelihood of her losing her leg, said Dr. Shuster.
Dr. Abdulrehman and Dr. Shuster worked collaboratively on Roy’s case. The procedure required two “kissing stents”, to be simultaneously and precisely placed – one by each specialist -- abutting each other and perfectly balanced at the spot where the aorta branches off into the two arteries bringing blood to her lower limbs. At the same time, they had to ensure the inserted stent didn’t block a third artery that had been surgically constructed to flow blood to the transplanted kidney, her only working kidney, and which branched off one of the bilateral arteries. The measurement and placements had to be very precise.
The procedure was a success and Roy is now back in Nakina, safe and whole.
“There’s no comparing what my life would be without (my leg),” she said. “It’s very important to have this service here.”
The specific benefit to Roy is obvious. But developing a cardiovascular service in Northwestern Ontario will have a tangible benefit for the entire region, said Arlene Thomson, Program Director, Cardiovascular and Stroke. This region has the worst health status in the province. People here are at increased risk of developing vascular complications due to a variety of factors, including a higher rate of diabetes.
“The loss of a limb is extremely devastating and changes lives,” said Thomson. “Patients lose their independence, often their ability to earn a living and also face high risks related to the progression of other cardiovascular diseases. The fact that we can now offer our patients the best options available will help us reduce amputation rates. The benefit of saved limbs for our patients, their families and society in general is immeasurable, but it is obviously very real and dramatic.”

Members of the vascular team after a recent kissing stents procedure. From left, Dr. Anatoly Shuster, Interventional Radiologist, Dr. Yaasin Abdulrehman, Vascular Surgeon, Rebecca Smith, Medical Radiation Technologist and Christy Laatu, Medical Radiation Technologist.
Easing the Pain: New Comprehensive Pain Management Program
Of all the symptoms patients experience while in hospital, pain may be the most distressing. Not only can it delay recovery from surgery and discharge home, the pain may persist for months or years.
“Appropriate pain treatment can be difficult to obtain and challenging to administer. In our Strategic Plan 2020, we have committed to enhancing the delivery of our clinical services – and that includes pain management,” explained Dr. Ian Dobson, Chief of Anesthesia. “Thanks to funding from the Ministry of Health, we’ve launched a Comprehensive Pain Management program which will deal with both acute and chronic pain and hopefully address some of these shortfalls.”
The chronic pain management component is mainly an outpatient program run through Ambulatory Care. Initially set up to assess and treat chronic back pain, the service will expand to manage other types of chronic pain syndromes.
“Treatments may include nerve blocks, pharmacologic therapy and other more novel forms of treatment such as radio-ablation and lidocaine infusions,” said Dr. Dobson. “Previously, chronic pain patients had to travel out of town for assessment and treatment, and wait lists were in excess of one year with little or no follow-up available. This is a service which is long-overdue for our region and our hope is that as the local demand grows, we will be able to recruit other interventional pain specialists and expand to handle all chronic patients locally.”
The new service is also building bridges with the behavioural pain management program at St Joseph's Care Group supporting a holistic approach to this complex problem.
The other arm of this comprehensive pain program is the Acute Pain management service which is designed to manage short term post-operative pain. This service will involve all members of the Anesthesia department and provide daily assessment and treatment plans as well as 24/7 on-call coverage to implement optimal pain management strategies. A pain management nurse will assist with assessments and visit patients daily, under the direction of the Pain Service physician.
“The goal is to optimize pain management employing currently available modalities such as patient controlled analgesia (PCA) pumps, epidural infusions and multimodal pharmacologic therapies,” explained Dr. Dobson. “When acute pain is managed effectively it not only improves patient satisfaction and comfort, it also allows them to concentrate on their rehabilitation and other important aspects of their recovery.”
Studies have shown that appropriate management of acute pain is a key factor in avoiding the development of chronic pain syndromes. Ensuring our patients are as healthy and comfortable as possible is part of Patient and Family Centred Care, the integral philosophy of our organization.

Dr. Ian Dobson, Chief of Anesthesia, TBRHSC, adjusts the settings on a PCA (Patient Controlled Analgesia) pump. This equipment helps to optimize pain management, which ultimately improves patient comfort and satisfaction.
Seniors' Health
Enhance the care provided to an aging population.
The population of seniors is growing. Baby boomers' health care needs will continue to increase. We recognize that the care needs of seniors are different, and will tailor services to accommodate them.
To advance care for the aging population, we will focus on these Goals within Seniors' Health:
- Deliver an optimal experience for seniors;
- Adopt the Ontario Senior Friendly Hospital Framework.
We will know we are successful by 2020 when we demonstrate:
- Seniors' hospital experience is optimal;
- Seniors and their families are highly satisfied and engaged in care.
We have made progress in this area already. These stories are examples of initiatives that are underway.
Improving Care for Elderly Patients: HELP Drastically Reduces Delirium Rates
Primarily a delirium prevention program, the Hospital Elder Life Program (HELP) maintains cognitive and physical functioning, maximizes independence at discharge, reduces hospital stays, and reduces readmission rates for senior patients.
Delirium Screening: A Step Toward Optimizing Senior Care
A pilot project for delirium screening is helping address the special.
Improving Care for Elderly Patients: HELP Drastically Reduces Delirium Rates
Drastically reduced rates of delirium and improved experiences for senior patients. These are some of the successes of the Hospital Elder Life Program (HELP) at Thunder Bay Regional Health Sciences Centre.
“It’s primarily a delirium prevention program, but HELP also maintains cognitive and physical functioning, maximizes independence at discharge, reduces hospital stays, and reduces readmission rates,” explained Kelsey Lecappelain, HELP Coordinator. Delirium is a sudden onset of confusion and can be brought on by a number of factors associated with lengthy hospital stays.
“Since we launched just over a year ago, HELP (in a select population) has reduced average elderly hospital stays from 12 to 7 days, reduced delirium rates from 10% down to 1%, reduced the number of senior patients discharged to long-term care from 10% down to 1%, and prevented mental and functional decline in older patients while maintaining their dignity and respect,” said Lecappelain.
A registered, comprehensive program of care for hospitalized older patients, HELP uses a team of well-trained volunteers who visit patients daily and provide therapeutic activities and games, walking or exercise, and help with feeding. Dedicated HELP volunteers have collectively provided over 2,100 hours of quality time with patients.
“The volunteers were there when I needed to talk. HELP is an excellent program and I am very happy it’s being implemented,” stated a previous HELP patient. “This is a great program for my mother,” said another patient’s family member. “The volunteers are friendly and great for my mother’s morale. Our family is extremely satisfied.”
Already, over 660 senior patients have been enrolled in the program. “HELP provides meaningful and cost-effective care that speaks loudly to our commitment to Seniors’ Health,” said Aaron Skillen, Program Director, Chronic Disease Prevention & Management and Medicine Services. “The program was designed from evidence and best practice, and clearly helps create an environment that minimizes the vulnerabilities of senior patients. It promotes comfort, safety, independence and functional well-being.”
Patients and families aren’t the only ones benefiting from HELP. Staff is also happy to have the program on their units. “We have received really positive feedback from staff, stating that their patients have been happier, they enjoy the interaction, and their cognitions have improved,” said Lecappelain.

Patients enrolled in HELP receive daily visits from dedicated, well-trained volunteers who help reduce delirium and improve the overall experience for senior patients. Above, a HELP patient welcomes a visit from Denver the Therapy Dog.
Delirium Screening: A Step Toward Optimizing Senior Care
Service demand is growing for senior patients. Baby boomers are quickly approaching an age where their demands on the health system will increase, affecting hospitals across Ontario.
At Thunder Bay Regional Health Sciences Centre, we recognize that the needs of senior patients are increasing, and also unique. To help address some of the special needs of senior patients, we’ve developed and successfully implemented a pilot project for delirium screening.
“Delirium is frequently overlooked or under-diagnosed due to multiple reasons, including limited staff knowledge about the detection, condition and prevention,” said Andrea Raynak, CNS Medicine, Interprofessional Education. “The Delirium Screening pilot project was very successful in implementing a new screening procedure that improves the level of care for our senior patients, and also in educating the staff on the preventative methods for delirium.”
The pilot project began with mandatory, interactive staff education which included overall information on delirium, preventative strategies and how to screen for delirium using the Confusion Assessment Method (CAM). This screening tool improves the identification and recognition of delirium. Nurses used the CAM screening tool within 48 hours of admission, and then daily on all patients aged 65 and over. If screening results are positive for delirium, the nurse would notify the most responsible physician.
“By increasing the level of attention given to senior patients, we can hopefully prevent delirium, or at least identify it early, resulting in an enhanced level of care from the beginning. This not only decreases staff workload, but creates a more optimal experience for senior patients and their families while decreasing staff work load,” explains Raynak.
The Delirium Screening pilot project was so successful that we continue to mandate daily screening of senior patients on the pilot unit. We believe the program has led to better patient outcomes by creating a safer environment, decreasing the length of stay and alternative long term care requirements for senior patients. The second phase of the project will see a delirium management procedure put into place to standardize delirium care and management for the senior population. It will also help to more accurately measure delirium rates and is expected to roll out by the end of Spring, 2016.
“As part of our Strategic Plan 2020, we are committed to providing an environment that minimizes the vulnerability of senior patients and promotes safety, comfort, independence, and functional well-being,” says Aaron Skillen, Program Director, Chronic Disease Prevention & Management and Medicine Services. “The delirium screening project is a great step towards delivering an optimal experience for seniors that is in line with Ontario’s Senior Friendly Hospital Framework.”

Andrea Raynak, CNS Medicine, Interprofessional Education, TBRHSC, screens a senior patient for delirium using the Confusion Assessment Method (CAM). By increasing the level of attention given to senior patients, staff can hopefully prevent delirium, or at least identify it early, resulting in an enhanced level of care from the beginning.
Indigenous Health
Enhance culturally appropriate care.
Indigenous people, particularly those from remote communities, face unique challenges to access to health care. In addition to geographical, language and cultural barriers, there are socioeconomic realities that simply do not exist outside of this population. Indigenous people account for at least 19% of our population. Unfortunately, they are the least healthy people in our region.
We aim to improve experiences and outcomes for Indigenous patients and families by providing care that is culturally relevant and sensitive, in welcoming environment.
Our Indigenous Health Goals are:
- Provide care that improves self-management, access, experience, and transition to home for Indigenous patients;
- Provide health care that respects traditional knowledge and practices, and builds TBRHSC as a leader in the provision of health care for Indigenous patients.
We will know we are successful by 2020 when we demonstrate:
- Indigenous patients from remote communities equally access, self-manage and transition to home;
- Indigenous people feel welcomed.
To monitor our progress we will measure the “Acute hospital admissions for patients from Indigenous Communities.” The data associated with this measure is new for us and will report results in 2016/2017.
Please read about recent activities in this area.
Helping Patients Heal with Smudging: Increased Access to Indigenous Spiritual Care
Recognizing that smudging is a major part of the healing process for many Indigenous patients, families and visitors, we now offer smudging on a regular basis.
Shaping Indigenous Health Through Engagement
The Indigenous Advisory Committee helps to improve experiences and outcomes for Indigenous patients.
Helping Patients Heal with Smudging: Increased Access to Indigenous Spiritual Care
A common tradition among First Nations, smudging involves the burning of one or more sacred medicines gathered from the earth: tobacco, sage, cedar and sweetgrass. Recognizing that smudging is a major part of the healing process for many patients, families and visitors, Thunder Bay Regional Health Sciences Centre now offers smudging on a regular basis.
“It’s a cleansing ceremony that can also be described as a different form of prayer, to either God or the Creator,” explained Reverend Michael Robinson, Spiritual Care Provider. “The smudge can help to calm and centre patients and visitors while they are at the hospital.”
Rev. Michael originally offered smudging to patients and their families once a week when he joined our team in April, 2015. Since then, demand has grown so high that he has increased smudging services to four times a week.
Regularly scheduled smudging takes place on Tuesdays and Thursdays, in both the morning and the afternoon and can be performed either in the specially ventilated Multi-Faith Spiritual Centre, or the Spirit Garden located in one of the hospital’s courtyards.
Personal smudges can be requested at any time. Rev. Michael performs an average of 16 individually requested smudges a week, and notes that people of all backgrounds and cultures are welcome to participate.
“It’s important that I remain accessible to patients and families whenever I’m needed, and I’m always happy to help in any way that I can,” said Rev. Michael. “I offer guidance to patients of any faith, but as a First Nations man, I specialize in Indigenous spiritual care. I think it’s especially comforting for our Indigenous patients that I’m also a Pipe and Eagle Whistle Carrier, because they know that means I have an understanding and awareness of their needs and concerns. It also helps that I’m always walking around smelling of smudge,” he joked.
Through his work, Rev. Michael is helping to grow a culture of awareness and understanding of Indigenous health. As awareness of his services grows, more people access them.
“We’re committed to providing health care that respects traditional knowledge and practices,” explained Tracie Smith, Senior Director, Communications, Indigenous Affairs and Engagement. “We have a long journey ahead as we continue to create an environment where Indigenous patients and families feel more comfortable. Ensuring access to a traditional practice such as smudging is an important step in that journey.”
Anyone interested in learning more about how to access smudging or other components of Indigenous culture and spirituality are welcome to contact Rev. Michael at the Spiritual Care office by calling 807-684-6235.

Reverend Michael Robinson, Spiritual Care Provider, prepares his smudge bowl in the serene, outdoor Spirit Garden at the Thunder Bay Regional Health Sciences Centre.
Shaping Indigenous Health Through Engagement
Indigenous people account for at least 19% of our population. Unfortunately, they are the least healthy people in our region. Those from remote northern communities in particular face unique geographical, language and cultural barriers to accessing health care.
We know this impacts overall health status, and have made Indigenous Health a priority for the next five years. We are committed to providing care that improves self-management, access, experience, and a safe transition home for Indigenous patients.
To improve experiences and outcomes for Indigenous patients, it is critical that Indigenous health activities are focused and impactful. The Indigenous Advisory Committee helps guide our actions and decisions.
“Access to quality health care is so important, especially for Indigenous people since we suffer from higher rates of chronic disease than non-Indigenous people,” says Robert Fenton, a representative of Ontario Native Women’s Association on the Indigenous Advisory Committee. “It’s encouraging to have a Health Sciences Centre that is committed to understanding our unique challenges and circumstances with regards to health care and I welcome the opportunity share my knowledge and experiences in the pursuit of solutions.”
The Indigenous Advisory Committee is comprised of external representatives of the organizations such as Nishnawbe Aski Nation, Matawa, Ontario Native Women’s Association, and Dilico Anishinabek Family Care, as well as community members. Experienced and dedicated committee members provide input on how to develop activities, and help monitor progress of the goals identified in our Strategic Plan as they relate to Indigenous Health.
“The Indigenous Advisory Committee is invaluable in terms of shaping and monitoring our progress in Indigenous Health,” said Tracie Smith, Senior Director, Communications, Indigenous Affairs and Engagement. “Their input ensures we are considering and addressing the unique needs of Indigenous patients and families, so that we can implement services and supports that are relevant.”
The Indigenous Advisory Committee has provided meaningful input on activities identified in the Strategic Plan 2020, including culturally sensitive ways to improve opportunistic screening for Indigenous patients, as well as approaches to recruit and support Indigenous volunteers. They have also provided recommendations to enhance a welcoming environment for Indigenous patients and families accessing care at our Health Sciences Centre.

Members of the Indigenous Advisory Committee share their knowledge and experiences to help improve Indigenous Health initiatives
Acute Mental Health
Enhance acute mental health service.
While Acute Mental Health inpatient days are decreasing at other hospitals, it has increased by 5.4% here. We want to be sensitive to patient needs, ensuring that mental health is viewed as part of overall health. We believe that everyone should be respected equally, regardless of age, illness or culture and will strive to provide a more holistic approach to treat the full human being – mind, body, and soul.
Within Acute Mental Health, we will:
- Adopt attitudes and behaviours that recognize mental health as an integral part of the delivery of comprehensive acute care services;
- Enhance the delivery of mental health care to patients outside of mental health services;
- Collaborate with system partners and appropriate governing agencies to develop and enhance transition in care;
- Enhance the delivery of ac te mental health care within mental health services.
We will know we are successful by 2020 when we demonstrate:
- The hospital supports a stigma-free environment;
- Access to Psychiatry service.

These stories provide examples of our commitment in action.
Connecting Patients to Urgent Mental Health Care
The Brief Intervention Treatment Team provides intervention for people who come to the Emergency Department in a mental health crisis.
Providing Increased Access to Mental Health Services
When patients with mental health challenges are admitted to a non-mental health unit, a new Mental Health Consultation Liaison Services provides assessment and treatment recommendations.
Connecting Patients to Urgent Mental Health Care
Mental health is a crucial component of health. That’s why acute mental health is one of the priorities in Thunder Bay Regional Health Sciences Centre’s Strategic Plan 2020. It’s a commitment to provide the best level of care for all mental health patients. This means ensuring that no patient falls through the cracks, and that each patient receives the care they need in a timely fashion. So, we’re expanding on an initiative that has proven to enhance experiences for mental health patients.
The Brief Intervention Treatment Team (BITT) includes professionals from psychiatry, psychology, social work, and nursing. BITT provides intervention for people who come to the Emergency Department (ED) in a mental health crisis but are able to remain out of the hospital if they’re given rapid outpatient follow-up. The team works closely with the Mental Health Assessment Team (MHAT) and the Adult Mental Health Inpatient Unit.
Our team continues to provide urgent treatment and intervention for people with mental illness who require immediate assistance or attention to help them avoid hospitalization. Patients no longer have to wait for referrals to psychiatric services. A member of the team can see the patient right away, which streamlines the process and improves outcomes for patients and families.
As we embark on our Strategic Plan 2020, the BITT program is evolving to the next phase of development.
There has already been a decrease in the number of admissions to Adult Mental Health, and a decrease in the number of short-term stays within Adult Mental Health. “We’ve seen a decrease in short-stay admissions to the unit because we’re able to connect patients to services right away,” explained Dr. Peter Voros, Program Director, Adult and Forensic Mental Health. “BITT has also helped improve the continuum of care by ensuring that connections are made for patients to appropriate long-term services in the community and that there is follow-up.”
“The initial goal of BITT was to facilitate timely mental health care for patients in the ED in order to avoid unnecessary admission to the Adult Mental Health Unit,” says Voros, “Moving forward for the next five years, providing quality urgent mental health care remains a top priority. As we enter the second phase of the initiative, we hope to expand the initiative with the ultimate goal of creating a full, separate emergency mental health space.”
While a separate emergency mental health space is expected to be approved by the year 2020, there is a lot of preparation that first needs to take place. Currently, our Adult and Forensic Mental Health team is focused on gathering as much information as possible and researching best practices. Soon, site visits of other well-functioning mental health emergency services will take place so that we can learn from the successes of our industry partners.

The Brief Intervention Treatment Team (BITT) includes professionals from psychiatry, psychology, social work, and nursing.
Providing Increased Access to Mental Health Services
Patients are physical, spiritual and mental beings. Sometimes, physical ailments can be accompanied by mental health issues. That’s why patients with mental health issues are often cared for in all areas of our Health Sciences Centre, and not only in acute mental health beds.
To increase access to specialized and appropriate Mental Health Services in all units, we are developing a new Mental Health Consultation Liaison Service. Through this service, patients with mental health challenges admitted to a non-mental health unit will be provided assessment and treatment recommendations.
“We want to be sensitive to all patient needs, and ensure that mental health is viewed as part of overall health,” explains Dr. Peter Voros, Program Director, Adult and Forensic Mental Health. “The Consultation Liaison Service will aim to provide timely mental health consultation for adult patients admitted to medical, surgical and critical care units within our Health Sciences Centre.”
The interprofessional consultation team will consist of psychiatry, mental health nursing and medical learners. Referrals will be made through the physicians providing care to patients who are experiencing symptoms of psychiatric distress while they are in hospital for a medical or surgical reason.
Once the service is up and running, patients would benefit from: referrals to psychiatric or behavioural management, liaison with the referring treatment team, ongoing monitoring of mental status during hospitalization, and facilitation of transfer to other mental health care services as required.
“This new service will help us enhance the delivery of mental health care to all patients, regardless of where they are in the hospital,” said Voros. “We believe this will be a significant step forward towards achieving our strategic goals of increasing access to specialized and appropriate mental health services on all in-patient units, and developing clear treatment plans for mental health patients outside of mental health beds.”
As part of our Patient and Family Centered Care philosophy, the Consultation Liaison Service will also provide assistance and support for the family members of patients. This multi-disciplinary approach will ensure that patients and families are receiving the right care, at the right time, in the right place.

The new Mental Health Liaison Service provides assessment and treatment recommendations for patients with mental health challenges admitted to a non-mental health unit. The interprofessional consultation team consists of psychiatry, mental health nursing and medical learners.
Your Donations Make a Difference
Overall in 2015, 26 grants, totaling $2,886,956 were distributed throughout the Thunder Bay Regional Health Sciences Centre and to several hospitals across Northwestern Ontario. Some of the significant equipment purchased, thanks to donors, was a new ultrasound unit and breast MRI coil in Diagnostic Imaging, ventilators for our Intensive Care Unit and significant support for research taking place at the Thunder Bay Regional Research Institute.
Donors continue to make a tremendous impact at the Health Sciences Centre. From gifts made to celebrate special occasions, to memorial gifts, to gifts made through a Will, donors have shared their enthusiasm for health care that is second-to-none, here at home.
Thunder Bay Regional Health Sciences Centre belongs to the community it serves and has always relied on the generosity of the community to ensure the care provided here is world-class. Just as the Health Sciences Centre belongs to the community, so does the Thunder Bay Regional Health Sciences Foundation. It exists to serve donors to ensure their passions and dreams come to life through gifts made in support of the Health Sciences Centre.
A full listing of grants made possible thanks to donors in our community is available at: healthsciencesfoundation.ca/impact
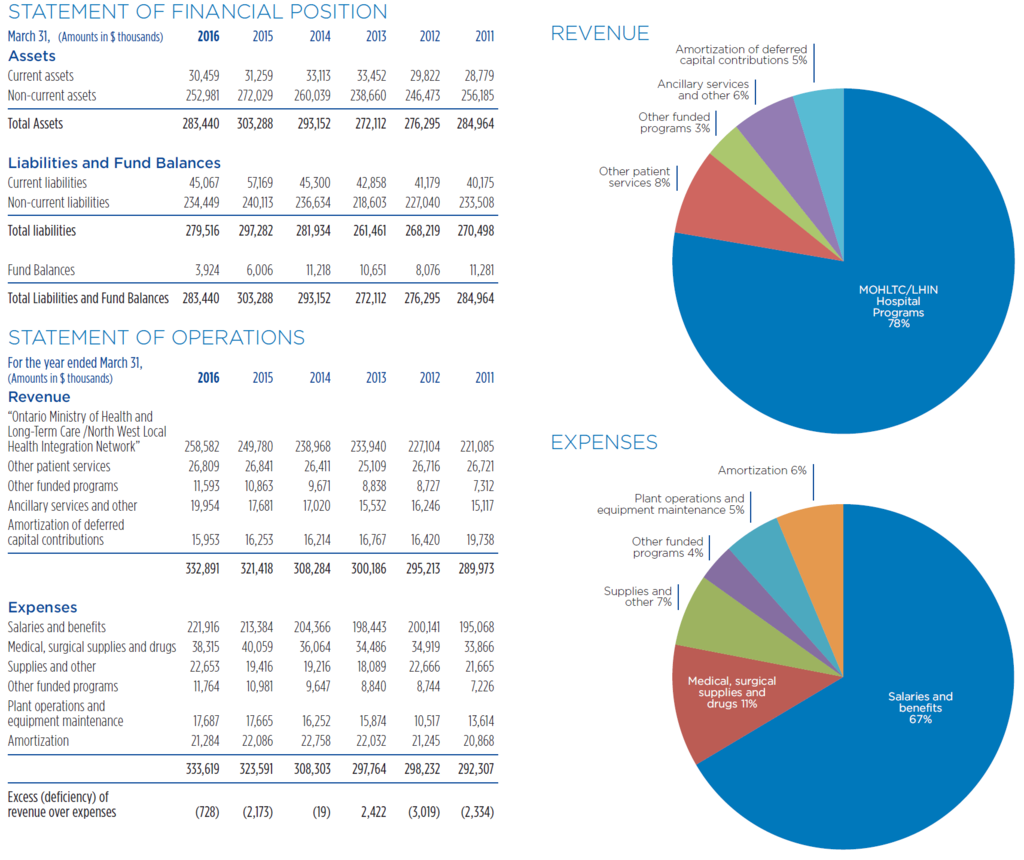
Financial Statements
Thunder Bay Regional Health Sciences Centre efficiently provides quality acute health care for the residents of Northwestern Ontario. Despite ongoing efforts and commitment to quality, effectiveness and efficiency, our Health Sciences Centre continues to face service and financial pressures as a result of many fiscal, demographic and health care system challenges. In 2015-16, we faced financial pressure because we were regularly in surge capacity, which occurs when there are more patients in the facility than the funded beds available. Our budgeted deficit for 2015/16 was greater than $5 million. We received one-time funding from the North West Local Health Integration Network and the Ministry of Health and Long Term Care to address a majority of the deficit. We continue to work closely with the Local Health Integration Network and other community partners to address the ongoing challenges.