Compre-
hensive
Clinical Care
Enhance the delivery of our clinical services.
Comprehensive Clinical Care
Enhance the delivery of our clinical services.
Comprehensive Clinical CareWe will deliver a quality patient experience in an academic health care environment that is responsive to the needs of the population of Northwestern Ontario.
Patient and Family Centred Care is the philosophy that guides us. Patients and Families are at the centre of everything we do.
We will focus our efforts on Patient Experience, Seniors' Health, Comprehensive Clinical Care, Aboriginal Health and Acute Mental Health.
Patients ARE First:
Patients and families at the centre of everything we do. At our acute health care facility, we provide care to the people of Northwestern Ontario - a region the size of France.
Ours is the teaching hospital of choice for over 1,500 learners from the Northern Ontario School of Medicine, Lakehead University, Confederation College, and other partnering academic institutions. We are an academic health sciences centre, committed to teaching the next generation of health care providers and advancing medical research. Patients benefit from interprofessional teams of healthcare providers and access to leading-edge medical equipment and clinical trials.
Providing effective health care for patients and families has earned us both Innovation Awards and Leading Practice Designations. We are a national leader in Patient and Family Centred Care.
The Health Sciences Centre belongs to the community it serves; the 250,000 residents of Northwestern Ontario. Our Strategic Plan 2020 was built by and for them.
We are pleased to provide this report on the 2018-2019 fiscal year progress of the Strategic Plan 2020.

As a community member and a client of health care services in Northwestern Ontario, I am excited about the opportunities presented by Ontario Health Teams (OHT). OHTs are intended to bring together Health Services Providers (HSP) serving a geographically defined population. The OHT will be clinically and fiscally accountable for delivering a coordinated continuum of care. Through this model, patients will be cared for, even if they’re not in the same organization or physical location. The goal is to provide better, more integrated care. OHTs are expected to enhance patients’ health care journey through flawless transitions in care, improved access to online health records, and a clear accountability framework.
Northwestern Ontario is well prepared for this project. When the call for Readiness Self-Assessments was issued in April, more than 30 Northwestern Ontario network HSP leads from multiple sectors, including our Hospital, put pen to paper highlighting this region’s strong history of partnership, collaboration, and innovation in identifying and meeting the health care needs of Northwestern Ontario residents. The Ministry of Health and Long-Term Care has acknowledged receipt of our submission. A decision is expected in June whether Northwestern Ontario has been selected to proceed to an application to be designated as an OHT.
The concept of improved integration of health services to enhance patient journeys and care outcomes is being discussed throughout the province. It was the primary topic of the Rural and Northern Health Care Leadership Conference hosted by the Ontario Hospital Association; the Hospital President & CEO, Jean Bartkowiak, and I attended that conference on May 7 and 8 in Toronto. The annual conference brings together board members and senior leaders from small, rural and northern health care organizations, to learn and explore strategies to address significant health system challenges and emerging trends impacting isolated HSPs. The program focused on building healthy communities; a transformation imperative for hospitals and community partners. We also explored the opportunities and important drivers for effective patient partnership to ensure the patient voice is incorporated in policy and program decisions, as well as care delivery and quality improvement processes. Learnings are highly relevant to our next steps as health care providers in Northwestern Ontario as we determine how to best collaborate to provide a coordinated continuum of care for patients.
In the same spirit of coming together to affect positive change, donations made to the Hospital Foundation have a significant impact to patients and families. The Ibn Sina Simulation Lab was generously funded through a $500,000.00 donation by the Muslim Physicians Group. The Simulation Lab advances our academic mission by enabling learners at the Hospital to enhance their skills through ongoing education using simulation. Current and future learners will pass those benefits on to our patients and their families through safe, quality patient care. This significant gift will continue to enhance experiences for patients, staff and learners well into the future. Our sincere gratitude is extended to these physicians who continue to role model the dedication and action required to advance safe quality patient care.
I am very proud of the entire Hospital team, staff, professional staff, scientists, learners, volunteers and donors, whose combined engagement and commitment result in continuous progress toward our Mission and Vision. I encourage all members of the community to review the 2018-2019 Annual Report of the Hospital and Health Research Institute. The report will be available June 21 at www.tbrhsc.net, following the Annual General Meetings of the Boards of Directors of the two organizations. This year’s Annual Report will provide an overview of some of the initiatives, improvements, learnings and discoveries in our delivery of patient care, teaching, and research.

Matt Simeoni, Chair, Thunder Bay Regional Health Sciences Centre Board of Directors

This past year, Thunder Bay Regional Health Sciences Centre achieved many accomplishments guided by our Strategic Plan 2020 and its five Strategic Directions (Patient Experience, Comprehensive Clinical Care, Seniors’ Health, Indigenous Health and Acute Mental Health). The successes contributed to the delivery of quality patient care and improved patient flow – ensuring patients access the right care, at the right time.
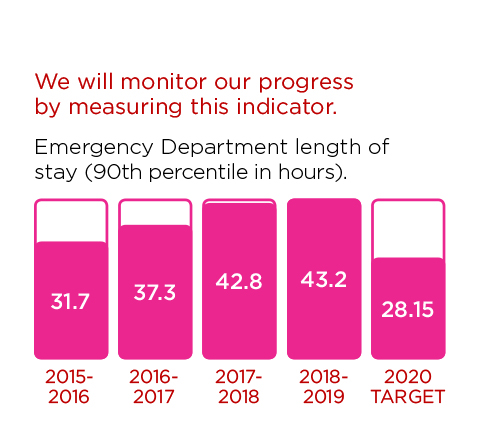
Improving patient flow continues to be one of our main challenges; indeed, over the years we have seen regular increases of inpatient admissions up until 2018-19, the first year where we experienced stabilization. It is still early to boast we are succeeding, but we think that several initiatives introduced in the last year have led to avoided admissions, improved patient journey at the Hospital, from admission to discharge, while maintaining safe, quality care and patient satisfaction. Patient flow remains as one of the largest issues affecting our Hospital, however our Emergency Department (ED) (where a very significant fraction of our patient admissions occur) is becoming less busy, which could also impact our overall admission rate. Furthermore, the examples below describe some of the progresses within each Strategic Direction that contributed to improved patient flow.
A new computerized bed report has made significant improvements by providing efficient and detailed bed occupancy reports in real-time, which allows members of our health care team to better track patient occupancy and address potential service delays for patients in a more timely and accurate way. This new system is a foundational change that sets the stage for upcoming patient flow improvement strategies and initiatives.
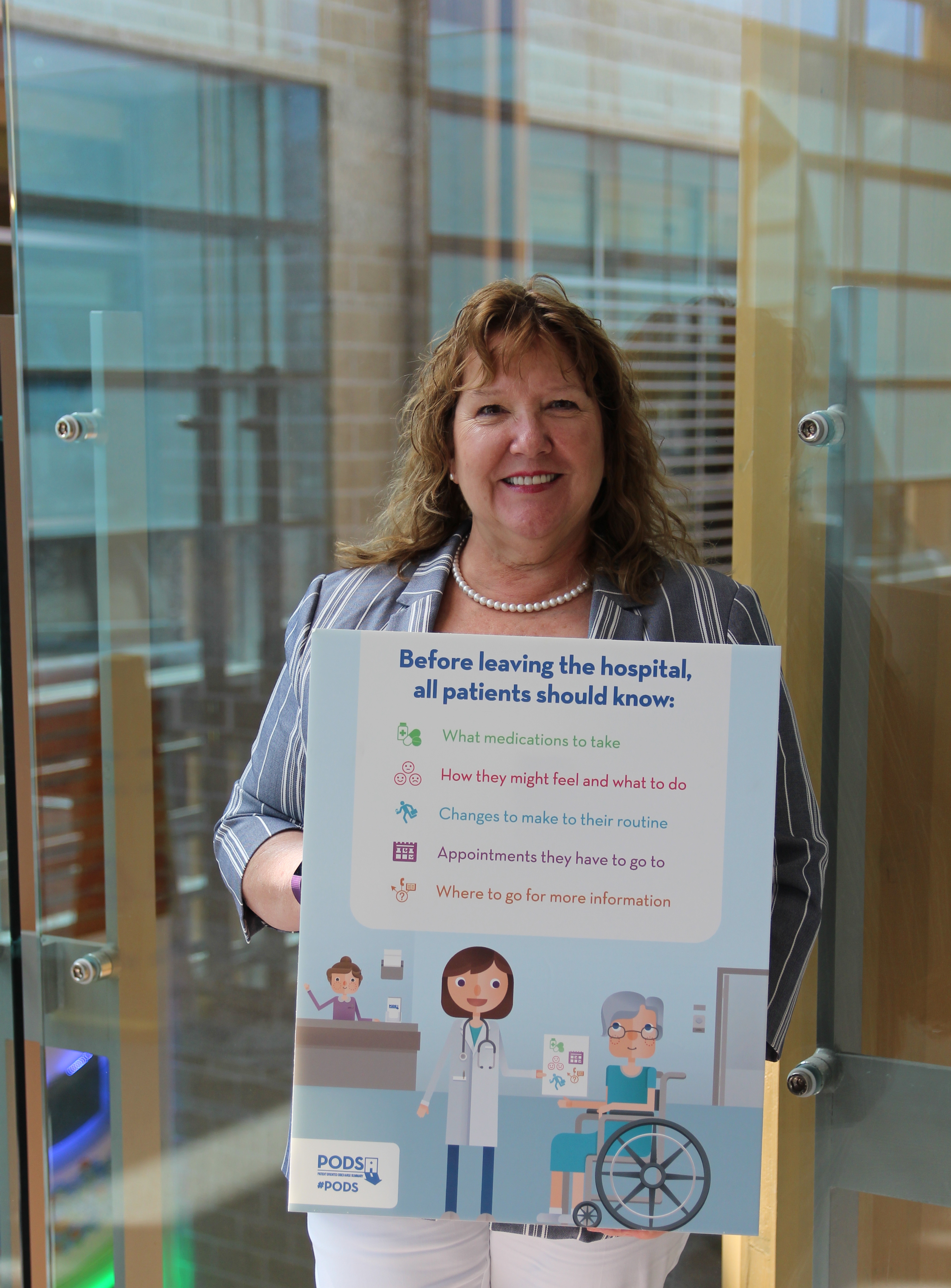
Patient Oriented Discharge Summaries (PODS) have now been implemented Hospital-wide. Co-developed by patients and health care providers, PODS improve the discharge process and help patients better manage their post-hospitalization care by providing them with clear and easy-to-understand instructions upon discharge. A true example of Patient and Family Centred Care, the tool ensures a smooth transition from hospital to home, which is an important part of the overall patient journey.
Senior patients at our Hospital are receiving the right care, at the right time, and by the right provider thanks to expanded coverage for the Geriatric Assessment program. Beginning whenever frail elderly patients arrive in the Emergency Department, the specialized staff assigned to the program identify the needs of senior patients much sooner, which has helped reduce the average length of stay by half – meaning that vulnerable senior patients are not spending more time in the hospital than needed. Additionally, over 150 unnecessary hospital admissions have been avoided this year.
A new discharge planning collaboration was developed that successfully integrated Dilico Anishinabek Family Care Discharge Planners in our clinical teams. We are now pursuing formal partnerships with other Indigenous health provider organizations in order to expand and improve discharge planning for Indigenous patients.
An expanded Consultation Liaison Service provides hospitalized patients wherever they are in the Hospital with access to specialized and appropriate mental health care. The service refers patients to psychiatric or behavioural management and liaises with the referring clinical treatment team. The staff in this service also facilitate the transfer of patients to other mental health care services in our community whenever required, connecting patients to the care they need, when and where they need it.
You’ll read about these initiatives and more in this Annual Report.
We are on track to meet our remaining Strategic Plan 2020 commitments. Our successes would not be possible without the dedication of our talented staff, physicians, researchers, volunteers and donors. Their commitment to our Patient and Family Centred Care philosophy and improved patient journey is truly remarkable
Thank you for contributing to our vision of aspiring to be healthy together.
Thank you.
Jean Bartkowiak
President & CEO

President & CEO

Many times during the year I find myself in conversation explaining to someone or a group how it is that our Hospital has a true partnership with patients through our Patient and Family Advisor (PFA) program. Even though the PFA program is now 10 years old, not everyone understands how much input PFAs have. We help make every major decision at the Hospital from hiring executives to creating policy. The list of projects that patients and staff have worked on together is astounding.
What jumps out at me though are the effects this partnership has on reaching the goals we set out in our Strategic Plan 2020. The strategic plan is our guide and roadmap to how we are going to deliver health care services to our regional patients. Without this plan, we would be like a ship without a rudder.
I’m happy to report that our completion rates for the goals in our strategic plan are some of the highest in the province. We have learned that the more we engage our patients at all levels, the greater our results will be. The input of PFAs improves policies, helps make health care programs more patient- and family-centred, and in turn leads to better outcomes for patients.
The strategic plan is a good example of something very important that starts in the boardroom and works its way to direct care at the bedside, and how PFAs enhance that care along the way. Personally, I feel a sense of pride knowing that every area of that plan was developed and improved thanks the partnership between the Hospital, our patients, and our community. We have developed such a strong working relationship, and a lot of hospitals around the country come to us to learn how to bring Patient and Family Centred Care (PFCC) into their own hospitals.
Congratulations to our staff, professional staff, volunteers, PFAs and donors again this year for their hard work and dedication. We are all true partners in our goal to live “Healthy Together”.
Thank you.

Co-Chair, Patient and Family Advisory Council

First, thank you to Dr. Gordon Porter, who was Chief of Staff at the Thunder Bay Regional Health Sciences Centre for almost a decade when he stepped down on October 31, 2018. Among other things, he led the work on our STEEEP (Safe Timely Efficient Effective Equitable Patient and Family Centred) quality framework. His leadership was an asset for our Hospital, and he was a tremendous mentor for me as I took on the role of Chief of Staff on November 1. Most of the following successes in this report are a continuation of Dr. Porter’s efforts.
I am happy to report that on January 9, 2019, our Hospital was awarded a Leading Practice Designation for our Patient Advisor, Cathy Pilot as a member of the Medical Advisory Committee (MAC). Cathy has brought the patient perspective to the MAC for over three years, providing invaluable input to help guide decisions in areas of patient care and improving patient flow.
One of those areas is our Length of Stay metrics, and we have added a few more initiatives to our work plan. We will use the guidelines from Choosing Wisely Canada, the national voice for reducing unnecessary tests and treatments. Not only are unnecessary tests unhelpful, they can actually harm patients through stress, false positives, and other negative consequences. Avoiding needless procedures can also reduce wait times for patients and costs to the system. Currently, we have submitted an application to become a designated Choosing Wisely Canada site.
Our Hospital has made great strides improving some very important wait times including for Cataracts and Joints, which are exceeding provincial benchmarks. We are also successfully meeting expected times to treatment for stroke patients, and we are third in the province for time to catheterization for patients with heart attacks requiring angioplasty.
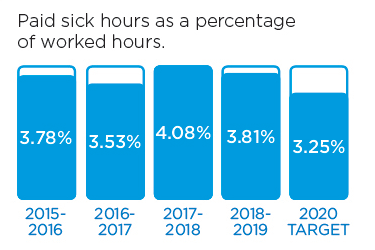
Staff burnout is an increasing challenge that impacts patient care. Last year, we added Professional Satisfaction to the Institute for Healthcare Improvement Quadruple Aim along with Better Health, Better Care and Lower Cost. A survey in November 2018 found that Professional Staff Engagement increased by 15% and that we had improved in 29 out of 32 areas since 2015.
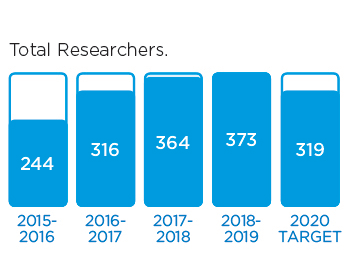
We continue to promote education and research as an academic health sciences centre. This past year, our Hospital hosted over 350 medical learners, over 500 nursing learners, and over 100 learners from other disciplines. We also have over a 150 physician-led research projects at the Hospital.
I am extremely proud of the professional staff who provide safe, timely, efficient, effective, equitable and patient-centred care to the people of Northwestern Ontario every single day under tough circumstances and with limited resources. We continue to work together to achieve improved patient satisfaction and outcomes by providing the Right Care at the Right Time in the Right Place by the Right Provider.
Thank you
S. Zaki Ahmed, MD, FRCPC, FCCP, CCPE, MHSc (Health Admin)
Chief of Staff
Chair, Medical Advisory Committee
We are leaders in Patient and Family Centred Care (PFCC), and it is the philosophy that guides us. We recognize that creating a quality patient experience builds upon this philosophy.
We are focused on enhancing the Patient Experience as one of our strategic priorities. Our goals are to:
We will know we are successful by 2020 when we demonstrate:
These stories provide an insight into three of the many Patient Experience initiatives last year
Strong leaders build strong teams that can accomplish the best results. For Thunder Bay Regional Health Sciences Centre, that means the best possible outcomes for patients and families. What separates high performing teams from dysfunctional ones is the way teammates treat one another. That’s why our Hospital is focused on leadership development and psychological safety.
Psychological safety is achieved when team members feel safe to take risks and be vulnerable in front of each other. Behaviors that create and maintain a level of psychological safety in a group support people to feel comfortable to fully contribute, which enhances the group’s potential.
The focus on psychological safety is part of the ‘Me to We to All’ leadership framework that was developed in earlier stages of the Strategic Plan 2020. It’s a comprehensive approach to leadership that focuses on improving the organization’s culture from the top down.
“We have to focus on staff-centred leadership as part of Patient and Family Centred Care – treating staff the way we want them to treat our patients,” said Amanda Bjorn, Executive Vice President of People, Culture and Strategy. “One of the main principles is helping leaders to better understand themselves and how the ‘me’ affects the ‘we’. It’s about focusing on people’s unique and individual strengths, and learning to use them in a positive way for the benefit of the whole team. We also explore our weaknesses, or our ‘leadership shadows’, so that we can better understand our impact on others both positively and negatively.”
The coaching approach to leadership has been shown to build psychological safety. Ultimately, the goal is that the Hospital’s coaching approach will guide all interactions at the Hospital – both among colleagues, and with patients and families.
“There are megatrends that influence and dictate the leadership styles that will be required for success into the future,” said Bjorn. “We are shifting to a coaching, collaborative, and co-creative approach when working with each other and will continue to deepen this in our interactions with our patients.”
The LIFT team members (Leaders Influencing the Future Today) were the first to experience coaching with an emphasis on psychological safety; and have begun a formal coach training program (The Business Coaching Advantage TM program) to enhance and strengthen their coaching skills. The experience supports them to personally understand the benefits of coaching and accelerate their leadership journey. Moving forward, the training cycle will continue until most members of the leadership team have had a chance to be coached, be the coach, or even receive formal coach training.
“Coaching is often misunderstood as something punitive; but I want everyone to know that coaching is actually a personal growth acceleration tool that deeply benefits our high performing leaders who want to enhance their strengths and take their leadership to the next level,” said Bjorn.
The process is still in the early stages and Bjorn is encouraged by the positive feedback received. “Our leaders have welcomed the coaching process so far. We’re creating a space where our leaders can grow together and feel confident in sharing their thoughts and suggestions for improvement. I’m encouraged for the future and the impact this will have on our staff and our patients and their families.”

The LIFT (Leaders Influencing the Future Today) team was among the first group of Thunder Bay Regional Health Sciences Centre leaders to undergo leadership coaching with a focus on psychological safety.
A smooth transition from hospital to home is an important part of the patient journey. Thunder Bay Regional Health Sciences Centre has implemented a special tool across all medical units that improves the discharge process and helps patients better manage their post-hospital care.
The Patient Oriented Discharge Summary (PODS) was co-developed by patients and health care providers and applies best practices in design and adult learning. Patients receive a set of clear and easy-to-understand instructions upon discharge including when to take their medication, what symptoms to be concerned about, and when to see their doctor next.
“For some patients and their families, the process of leaving the hospital and figuring out how to manage their condition from home can be stressful,” said Bonnie Nicholas, Acting Senior Director of Quality and Risk Management. “PODS was developed with the patient and family needs in mind, provides the valuable information that they want, and helps ensure their safe transition to home.”
One of the best qualities about PODS is that they are tailored to each patient and their specific condition. For example, patients with congestive heart failure are provided with information that includes a list of possible symptoms to watch out for and their correlated severity and cause for concern, along with next steps to follow if they are experienced.
“Our goal with implementing PODS across the Hospital was to improve patient confidence and their overall experience once they leave the Hospital,” said Nicholas. “Patient surveys have shown that PODS has been successful and our patients are very happy with the quality of information they are receiving. It’s a great tool that builds upon our Patient and Family Centred Care Philosophy.”
In addition to improving patient satisfaction rates, PODS also has a positive impact on patient outcomes. Since patients are leaving the Hospital with a better understanding of their health status, they are better equipped to adhere to their discharge instructions.
Our Hospital was able to successfully adopt PODS with support from ARTIC (Adopting Research to Improve Care), a joint program of the Council of Academic Hospitals of Ontario and Health Quality Ontario. It was designed in collaboration with University Health Network’s OpenLab – a design and innovation group dedicated to finding creative health care solutions.
To learn more about PODS, visit www.hqontario.ca. To learn more about patient focused care at our Hospital, visit tbrhsc.net.
Bonnie Nicholas, Acting Senior Director of Quality and Risk Management
We aim to enhance the Comprehensive Clinical Care that transcends the organization and touches all patients. Our activities are focused on addressing gaps in care, so the people of Northwestern Ontario can receive quality care, closer to home.We aim to enhance the Comprehensive Clinical Care that transcends the organization and touches all patients. Our activities are focused on addressing gaps in care, so the people of Northwestern Ontario can receive quality care, closer to home.
Within Comprehensive Clinical Care, we have identified the following Goals:
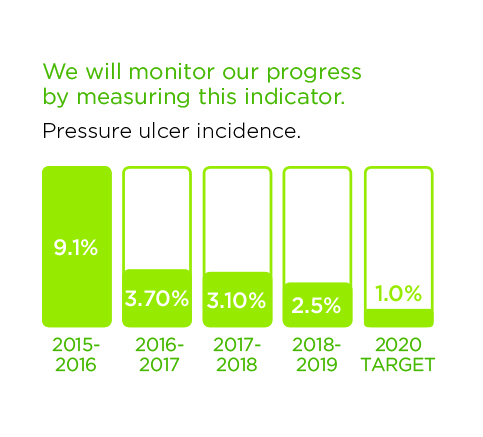
We will know we are successful by 2020 when we demonstrate:
Learn more about our exciting progress in this area:
We all know the importance of heart health, but what about your vascular system – the arteries and veins outside of the brain or heart? A new Rapid Access Vascular Examination (RAVE) clinic at Thunder Bay Regional Health Sciences Centre is raising awareness about the importance of vascular health, and significantly improving access to care for patients with potential vascular disease.
The RAVE clinic is designed for patients who have lower limb wounds such as foot ulcers and tissue loss that are not healing. In most people, such an injury will heal without difficulty within a week or two. However, when there is an underlying vascular problem, the tissue does not heal and requires a vascular assessment.
Patients of the RAVE clinic are typically seen within two weeks from the time of referral from their health care provider.
“For patients who are showing symptoms of vascular disease, the RAVE clinic provides specialized testing to assess their vascular health, and a vascular surgeon is available to perform further evaluation or develop a care plan,” said Arlene Thomson, Senior Director, Cardiovascular Program Development and Implementation. “The clinic really prioritizes vascular health, which is especially important in Northwestern Ontario where amputation rates are much higher than the rest of the province. Our ultimate goal is to reduce our region’s overall amputation rate by making vascular care more timely and accessible.”
All three of our Hospital’s vascular surgeons – Dr. Mary MacDonald, Dr. Elrasheed Osman, and Dr. Matthew Ingves - participate in the RAVE clinics, ensuring that patients have timely access to life and limb saving treatment. Depending on severity, patients can be treated through medical therapy, minimally invasive catheter procedures, or surgical reconstruction.
“In our region, we see a large number of patients presenting with prolonged lower limb wounds, which can be a sign of peripheral artery (vascular) disease,” said Dr. Matthew Ingves. “An early diagnosis can make all the difference in whether or not a limb can be salvaged and amputation avoided. The RAVE clinic is an excellent system for assessing patients in an efficient manner, while also increasing awareness about vascular health and its role in preventing amputations. We’re able to make a real difference by facilitating the best possible treatment for our patients and their families.”
If you have concerns about a lower limb wound that won’t heal or questions about your vascular health, please see your health care provider.

Dr. Matthew Ingves is one of three Vascular Surgeons at Thunder Bay Regional Health Sciences Centre providing timely access to vascular care through the Rapid Access Vascular Examination (RAVE) clinic.
Optimizing patient flow is about improving the care and resources needed to support patients throughout their journey at the Hospital, from admission to discharge. A new automated bed report at Thunder Bay Regional Health Sciences Centre is improving patient flow and helps patients receive the right care, at the right time.
“Patient flow remains as one of the most prevalent issues affecting our Hospital,” said John Ross, Director of Medicine, Patient Flow and Partnerships. “Our Emergency Department (ED) is one of the busiest in the province, and this, along with admission requests received from OR/Recovery Room, Outpatient Clinics, Regional hospitals and various home and community locations, means that we average approximately 60 admissions per day. Every improvement we make ensures that when patients are admitted they are able to move into an inpatient bed sooner.”
The newly created automated Patient Flow Report, implemented earlier in the year, is helping significantly to optimize the patient journey. This report provides efficient and detailed bed occupancy information in real-time, allowing members of the Hospital’s health care team to see and address potential delays in services for patients much sooner and with better accuracy.
“Before this improvement, bed reports were completed manually by the Admitting Clerks and this onerous task took valuable time away from the actual assignment of beds. When accounting for the ongoing demands of daily capacity and occupancy pressures, it is essential for our teams to be able to access relevant information in real-time to assist in the facilitation of patient flow,” said Nancy Saxberg, Manager of Corporate Patient Flow. “Our newly automated reports are much more efficient and accurate, and allow our teams to focus proactively on supporting patients to access beds when they need them.”
The creation of this new report is an important foundational change that sets the stage for more patient flow improvement strategies and initiatives. It has also significantly improved communication and coordination across all areas of the Hospital, as well as system partners across the region.
“It’s important to us that everyone in Northwestern Ontario who needs care can access it at the right time. Working together with health system partners is essential to ensuring that patients receive safe, quality care. The automated report supports us in doing that,” said Ross. “Patient flow improvement is a complex and ongoing strategy, and we are all committed to enhancing the coordination of care and working closely on a daily basis to support best possible outcomes and experiences for patients and their families.”

Thunder Bay Regional Health Sciences Centre’s Admitting Department is dedicated to improving patient flow. They work hard every day, supporting patients to access beds when and where they need them.
The population of seniors is growing. Baby boomers' health care needs will continue to increase. We recognize that the care needs of seniors are different, and will tailor services to accommodate them.
To advance care for the aging population, we will focus on these Goals within Seniors' Health:
We will know we are successful by 2020 when we demonstrate:
We have made progress in this area already. These stories are examples of initiatives that are underway.
Senior patients at Thunder Bay Regional Health Sciences Centre are receiving the right care, at the right time, and by the right provider thanks to expanded coverage for the Geriatric Assessment program.
Beginning in the Emergency Department, the program streamlines the assessment process of at-risk seniors (aged 65 years and older) through consultation with internal geriatricians and the Hospital Elder Lif> Program (HELP). Collaboration with external partners such as St. Joseph’s Care Group (SJCG), Alzheimer’s Society, Superior North Emergency Medical Service, and the North West Local Health Integration Network’s (LHIN) Home and Community Care, is also crucial to the program’s success.
“Senior patients often require more specialized attention within our health care system. In addition to requiring health care more often, their needs are different from the general population,” said Susan V>ltri, Geriatric Care Coordinator. “The Geriatric Assessment program is a great fit for their needs. After a successful trial of the program, we saw a need to not only make it a permanent service, but to expand coverage to seven days a week so that even more patients can be screened and as>essed.”
The assessment process looks for signs of geriatric syndromes, including mobility issues, weakness, frailty, functional decline, pain, cognitive impairment, dementia, delirium, and other risk factors often associated with seniors. “Early assessment allow for early interventions, which is especially crucial for at-risk seniors,” said Veltri.
The program also supports discharges for patients who do not require acute care in a hospital setting and works with community partners to provide a smooth transition to home or other programs and services that would best address their needs, such as SJCG’s geriatric programs.
By identifying their needs sooner, the average length of stay for senior’s of the program has decreased by half – meaning that vulnerable senior patients are not spending more time in the hospital than needed. Additionally, over 150 unnecessary hospital admissions have been avoide> this year.
“By providing senior-friendly care early, we reduce the number of unnecessary admissions or days spent in the hospital and achieve improved continuity of care, enhanced patient experiences and better outcomes,” said Veltri. “Most importantly, our senior patients and their families>and caregivers h>ve been very happy with the care received and the ongoing support provided after discharge.”
To learn more about our Hospital’s commitment to seniors’ health, visit tbrhsc.net.

The population of Northwestern Ontario is aging. As the senior patient population continues to increase, Thunder Bay Regional Health Sciences Centre is committed to providing them with an optimal experience in a safe and accessible environment.
The Hospital completed a physical environment gap assessment and in response, developed a physical environment plan that also aligns with the Hospital’s Accessibility priorities and goals. The plan was developed by a working group with input from Patient and Family Advisors to ensure the patient’s perspective was fully captured.
“Seniors’ Health is a priority within our Strategic Plan 2020 and we are committed to enhancing our environment to minimize the vulnerabilities of senior patients and promotes safety, comfort, independence, and functional well-being,” said Anne-Marie Heron, Executive Director of Capital Planning and Operations. “Although this work will be implemented over several years, our environmental assessment has already led to a number of improvements that are making our Hospital more accessible to senior patients and their families.”
Patients and visitors may have already noticed one of the improvements while using any one of the Hospital’s parking lots. New parking lot signs were installed that depict animal pictures and names, replacing the previous naming system of letters and numbers. The new signs are more visible with larger font sizes and the upgraded designation system makes it easier to remember where you parked.
Other improvements include adding more automatic door openers to the doorways in high traffic public areas and bathrooms – with future expansion to the patient units. The overhead clinical paging system is also being reviewed and will soon be upgraded in order to provide a quieter environment for patients.
“The physical environment component of a senior friendly hospital has a critical impact on the safety and functional level of senior patients,” said Heron. “We are committed to meeting the physical needs of our senior patients and their families in order to provide an optimal patient experience.”
For more information about how Thunder Bay Regional Health Sciences Centre is prioritizing Seniors’ Health and accessibility, visit tbrhsc.net.

Anne-Marie Heron, Executive Director of Capital Planning and Operations, along with one of the new and enhanced parking lot signs at Thunder Bay Regional Health Sciences Centre.
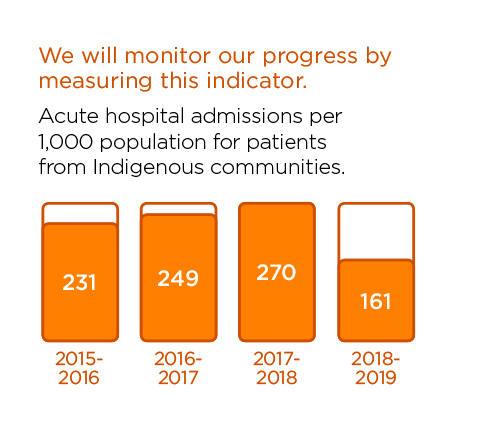
Indigenous people, particularly those from remote communities, face unique challenges to access to health care. In addition to geographical, language and cultural barriers, there are socioeconomic realities that simply do not exist outside of this population. Indigenous people account for at least 19% of our population. Unfortunately, they are the least healthy people in our region.
We aim to improve experiences and outcomes for Indigenous patients and families by providing care that is culturally relevant and sensitive, in welcoming environment.
Our Indigenous Health Goals are:
We will know we are successful by 2020 when we demonstrate:
Please read about recent activities in this area.
Cultural awareness, sensitivity, and respect contribute to positive patient experiences and outcomes. Thunder Bay Regional Health Sciences Centre is providing Indigenous cultural awareness education to staff, physicians and volunteers as part of our commitment to creating an environment where Indigenous patients and families feel more comfortable.
“Cultural awareness within health care helps create a safe space for open communication. When patients feel that health care providers respect their culture, they are likely to communicate more freely,” said Crystal Pirie, Senior Director of Indigenous Collaboration. “Our Hospital offers cultural awareness education so that we can provide care to Indigenous patients and families that is respectful of their diverse backgrounds, values, and traditions.”
Hospital leadership participated in an Indigenous trauma informed workshop that invited them to actively engage in a journey of experiential learning, self-exploration and awareness development. Audrey Gilbeau, Executive Director of Nokiiwin Tribal Council, lead the workshop and shared foundational teachings from Indigenous knowledge to enhance individual and organizational practices, and to foster trust and mutually respectful relationships based on shared values.
The Hospital also provides Indigenous cultural awareness education to all staff, physicians and volunteers as part of the Respect project. Initiatives include an online webinar and discussion-based team workshops that encourage people to challenge their own beliefs and biases through increased self-awareness.
“The training really gave me insight into Canada’s true history with regards to Indigenous people, the many impacts of colonialism and intergenerational trauma, and how those impacts still exist and impact our own personal biases and behaviours,” said Tracey Hill, Interprofessional Educator at the Hospital. “I walked away with knowledge that has opened my eyes and changed my perspective about the system we live and work in. As health care workers, this knowledge is especially important and will help transform our organization to be more understanding, and to treat all patients and families with compassion and empathy.”
Cultural awareness is valuable for health care professionals, health care organizations, and patients and families. Benefits include increased mutual respect between health care workers and patients, increased trust, and promotion of patient responsibility and empowerment in their own health care.
“Becoming culturally aware and sensitive is an ongoing journey and an important part of our commitment to provide health care that respects traditional knowledge and practices. The goal is to build our Hospital as a leader in the provision of health care for Indigenous patients and families,” said Pirie.
For more information about Indigenous health care at Thunder Bay Regional Health Sciences Centre, visit tbrhsc.net.
Indigenous people, particularly those from remote Northern communities, face unique challenges to accessing health care. Thunder Bay Regional Health Sciences Centre has a leadership position dedicated to improving experiences and outcomes for Indigenous patients and families by providing care that is culturally relevant and sensitive, in a welcoming environment, and also enhances partnerships to address challenges.
Crystal Pirie was hired as Senior Director of Indigenous Collaboration in August 2018. In this new role, she is responsible for meaningful engagement with Indigenous partners and communities, and advising the Hospital’s Senior Leadership Council and Board of Directors on strategies to enhance Indigenous health.
“My focus is to ensure our Hospital’s Indigenous Health priorities are authentic to the needs of the region’s Indigenous communities and that the Health Research Institute advances the health research priorities of Indigenous researchers and communities,” said Pirie. “Through collaboration with our internal teams as well as external partners and communities, I’m working to ensure that all of our Hospital’s policies, procedures and processes are more culturally relevant, sensitive, and holistic.”
Pirie oversees all of the goals and objectives that fall under Indigenous Health in the Strategic Plan 2020. One of her priorities this past year has been to gain a better understanding of who the Hospital’s Indigenous patients are in order to better determine their needs. Collaborating with regional partners, communities, and Federal and Provincial authorities is helping to map out the existing gaps in service – from a patient’s initial appointment through to their discharge.
In addition to the existing goals under Indigenous Health, a new strategic objective related to discharge planning was developed due to the success of the Dilico Anishinabek Family Care Discharge Planners. Under Pirie’s leadership, the Hospital will continue to pursue formal partnerships with Indigenous organizations in order to expand and improve discharge planning for Indigenous patients.
“There is certainly no easy solution to the unique challenges faced by Indigenous patients and families with regards to health care, but I’m encouraged by the commitment displayed by our Hospital to make positive changes,” said Pirie. “I’m proud to be the first point of contact for any questions or concerns from our Indigenous leaders and communities of Northwestern Ontario and look forward to building on those relationships. My goal is to see our Hospital become a leader in Indigenous Health.”
To learn more about Thunder Bay Regional Health Sciences Centre’s commitment to Indigenous Health, please visit www.tbrhsc.net/home/indigenous-health-services/.

Crystal Pirie, Senior Director of Indigenous Collaboration, hopes to see Thunder Bay Regional Health Sciences Centre become a leader in Indigenous Health.
While Acute Mental Health inpatient days are decreasing at other hospitals, it has increased by 5.4% here. We want to be sensitive to patient needs, ensuring that mental health is viewed as part of overall health. We believe that everyone should be respected equally, regardless of age, illness or culture and will strive to provide a more holistic approach to treat the full human being – mind, body, and soul.
Within Acute Mental Health, we will:
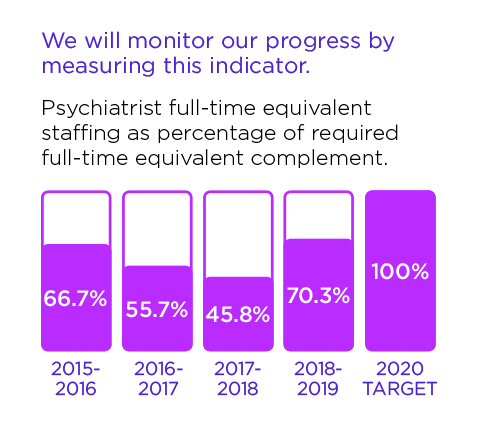
We will know we are successful by 2020 when we demonstrate:
These stories provide examples of our commitment in action.
Mental health is a crucial aspect of overall health. An expanded Consultation Liaison Service at Thunder Bay Regional Health Sciences Centre provides patients with increased access to specialized and appropriate mental health care.
The Consultation Liaison Service team refers patients to psychiatric or behavioural management, liaison with the referring treatment team, and provides ongoing monitoring of mental status. The team also facilitates transfer of patients to other mental health care services if deemed necessary. After proving successful during the pilot project phase, the service is now available to patients in all areas of the Hospital.
“We made a commitment to enhance the delivery of mental health care to patients outside of mental health services,” said Darcy Price, Acting Director of Adult and Forensic Mental Health. “This service helps us be more sensitive to patient needs by providing timely, efficient and robust mental health care for all patients, regardless of where they are located in our Hospital.”
The service also helps address the emerging substance abuse crisis that is happening across Northwestern Ontario. “We experience higher rates of substance abuse in our region, and people impacted can be patients of our Hospital,” said Price. “We are sensitive to all patient needs, and are strengthening the way we treat the whole human being – mind, body and soul.”
The Consultation Liaison teams consist of a psychiatrist and a mental health nurse. They connect patients, when necessary, to the appropriate community partners and agencies that can assist them on their continued path to healing. This includes connecting substance abuse patients to proper withdrawal management services and addiction counseling.
“We will continue to evaluate and enhance the service,” said Price. “Through ongoing engagement with our community partners and our internal nursing staff, we will identify any possible gaps in service and determine how we can further assist and support our patients and their families. It’s about being healthy together.”

Members of the Consultation Liaison Service from left to right: Dr. S Khalil, Psychiatrist, Dr. R Bismil, Psychiatrist, Erin Harasym, RN, Dr. D Wadhwa, Psychiatrist and Nadia Bottoset, RN.
A new mental health assessment process at Thunder Bay Regional Health Sciences Centre is improving mental health care for all inpatients outside of Mental Health units.
“Everyone has mental health, not just patients in our mental health units,” said Dr. Mandy McMahan, Director, Adult and Forensic Mental Health and Psychosocial Professional Practice Head. “Our strategic plan prioritizes mental health as an important aspect of overall health. Implementing this new assessment process across all inpatient units helps us provide crucial mental health care to all patients who may need it, regardless of where they are in our Hospital.”
The assessment is completed by a nurse on all patients once admitted to the Hospital. It incorporates the Patient Health Questionnaire for Depression and Anxiety (PHQ-4), an admission screening tool to help identify patients experiencing signs of mental illness. If a patient reaches a certain score, the nurse is prompted to notify the most responsible physician who will determine if a psychiatry referral or follow-up is required.
“Everyone experiences difficult times, especially when they are in the hospital. Building this assessment into our admission process makes it easier to determine whether or not a person is in need of mental health care and increases timely access to that care when it’s required,” said Dr. McMahan. “This tool helps to facilitate and normalize those important conversations regarding overall wellness. The purpose is not to assign a label to a patient; it’s about treating the whole person.”
The assessment tool creates a more standardized and proactive approach to helping inpatients at the hospital get the help they need for any mental health issue they are experiencing. With this process in place, more patients are getting the full spectrum of care that they need, when they need it.

Dr. Mandy McMahan, Director, Adult and Forensic Mental Health and Psychosocial Professional Practice Head
The Thunder Bay Regional Health Sciences Foundation connects a caring community to create better health care. Your donations to the Health Sciences Foundation support new medical equipment, technology and treatment programs in all areas of health care.
For the many patients served at the Thunder Bay Regional Health Sciences Centre each and every day, your donations are making a tremendous difference to the care we provide now and into the future. Every single department benefits from the generosity of donors – from our busy Emergency Department, to our Cancer Centre and Mental Health.
Of course, the need is constant. Health care is rapidly evolving, as are the services provided to patients in Northwestern Ontario. Right now our community is preparing to welcome a full-service cardiovascular surgery program that will revolutionize the care provided to approximately 1,000 patients a year.
It’s thanks to donors that our families, friends and neighbours have access to life-saving care closer to home.
For more information, including a full listing of grants made possible thanks to donors, visit: healthsciencesfoundation.ca
Since our region is unique in its health care needs and challenges, it makes sense that our research program would be unique as well. The Thunder Bay Regional Health Research Institute promotes patient-centred research that focuses on finding interventions and other procedures to solve health care challenges most prevalent in Northwestern Ontario – interventions and other procedures that also have global applications.
We encourage strong collaborations between our scientists and clinicians at the Thunder Bay Regional Health Sciences Centre and throughout the region to find homegrown solutions to the health care challenges that affect us most. The Health Research Institute follows the Council of Academic Hospitals of Ontario tenets of Healthier, Wealthier, and Smarter.
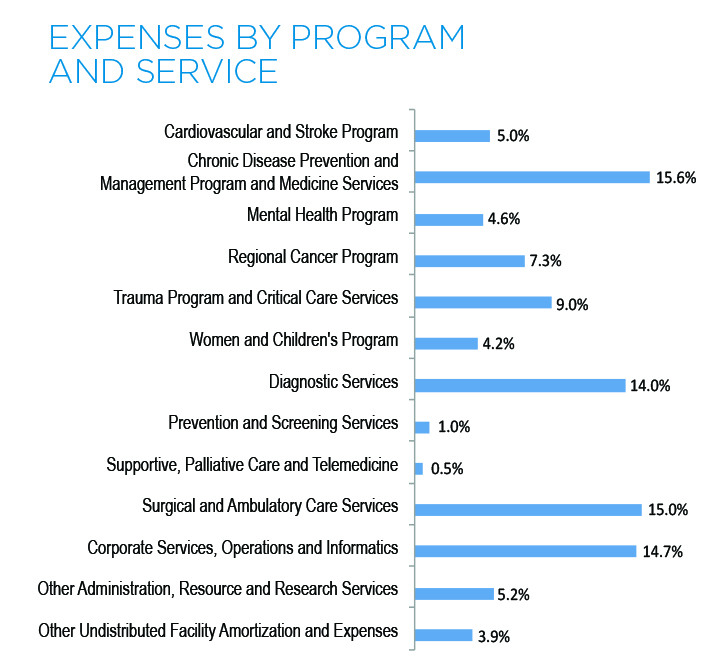
Thunder Bay Regional Health Sciences Centre continues to manage health care resources effectively and responsibly, while providing quality acute health care for the residents of Northwestern Ontario. Our Health Sciences Centre continues to face service and financial pressures as a result of many fiscal, demographic and health care system challenges. In 2018/19, we regularly operated in surge capacity, and this creates significant financial pressures. In addition to measures we took internally, we received one-time funding from the North West Local Health Integration Network and the Ministry of Health and Long Term Care to address some of the financial pressures. We continue to work closely with the Local Health Integration Network and other community partners to address the ongoing challenges.
(Amounts in $ thousands)
| For the year ended March 31 | 2019 | 2018 | 2017 | 2016 | 2015 |
|---|---|---|---|---|---|
| Assets | |||||
| Current assets | 35,600 | 38,085 | 29,125 | 30,459 | 31,259 |
| Non-current assets | 220,274 | 228,829 | 241,497 | 252,981 | 272,029 |
| Total Assets | 255,874 | 266,914 | 270,622 | 283,440 | 303,288 |
| Liabilities and Fund Balances | |||||
| Current liabilities | 51,682 | 51,236 | 46,199 | 45,067 | 57,169 |
| Non-current liabilities | 198,411 | 207,088 | 219,330 | 234,449 | 240,113 |
| Total liabilities | 250,093 | 258,324 | 265,529 | 279,516 | 297,282 |
| Fund Balances | 5,781 | 8,590 | 5,093 | 3,924 | 6,006 |
| Total Liabilities and Fund Balances | 255,874 | 266,914 | 270,622 | 283,440 | 303,288 |
| For the year ended March 31 | 2019 | 2018 | 2017 | 2016 | 2015 |
|---|---|---|---|---|---|
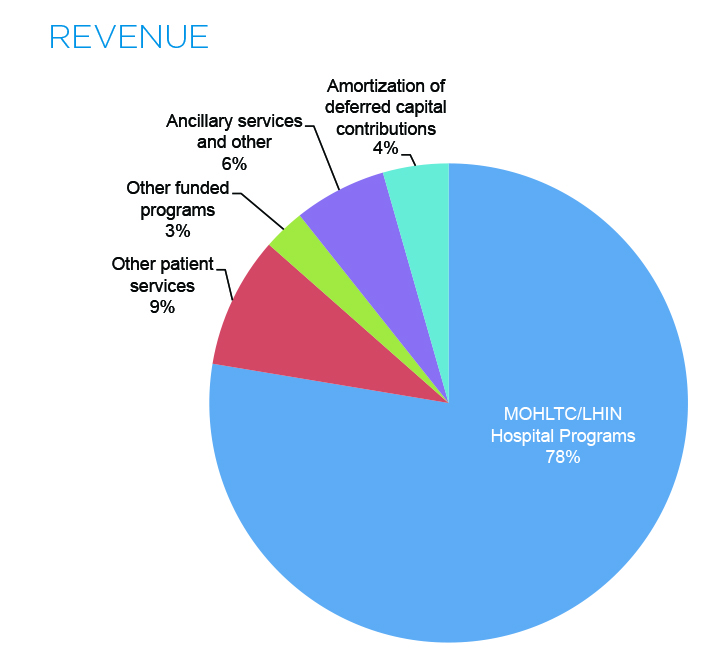
| Revenue | |||||
| Ontario Ministry of Health and Long-Term Care /North West Local Health Integration Network | 284,647 | 275,339 | 257,692 | 258,582 | 249,780 |
| Other patient services | 32,528 | 28,706 | 27,994 | 26,809 | 26,841 |
| Other funded programs | 10,342 | 7,689 | 7,693 | 11,593 | 10,863 |
| Ancillary services and other | 22,950 | 20,112 | 22,121 | 19,954 | 17,681 |
| Amortization of deferred capital contributions | 16,245 | 16,024 | 15,597 | 15,953 | 16,253 |
| 366,712 | 347,870 | 331,097 | 332,891 | 321,418 | |
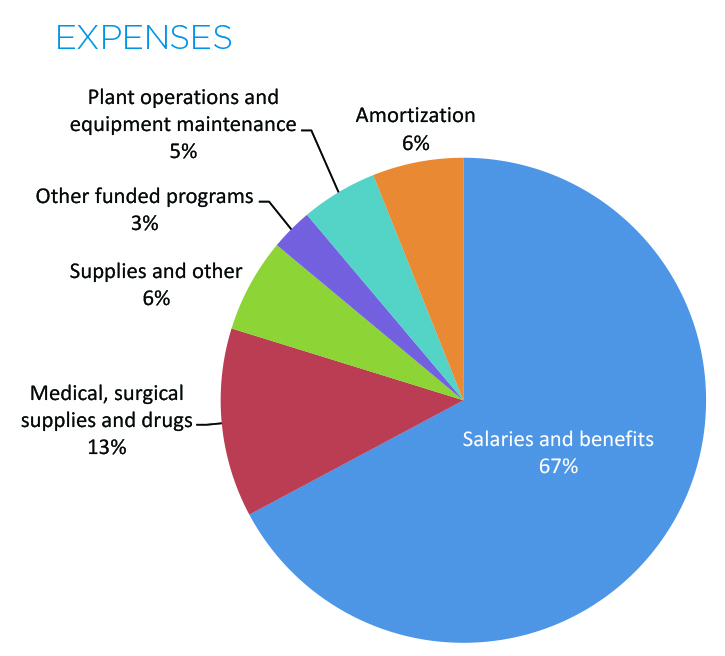
| Expenses | |||||
| Salaries and benefits | 247,682 | 233,900 | 223,589 | 221,916 | 213,384 |
| Medical, surgical supplies and drugs | 46,423 | 41,233 | 37,409 | 38,315 | 40,059 |
| Supplies and other | 23,095 | 22,834 | 23,386 | 22,653 | 19,416 |
| Other funded programs | 10,342 | 7,689 | 7,702 | 11,764 | 10,981 |
| Plant operations and equipment maintenance | 18,778 | 17,624 | 17,643 | 17,687 | 17,665 |
| Amortization | 22,300 | 22,384 | 21,818 | 21,284 | 22,086 |
| 368,620 | 345,664 | 331,547 | 333,619 | 323,591 | |
| Excess (deficiency) of revenue over expenses | (1,908) | 2,206 | (450) | (728) | (2,173)) |