Compre-
hensive
Clinical Care
Enhance the delivery of our clinical services.
Comprehensive Clinical CareThunder Bay Regional Health Sciences Centre
Our Vision
healthy
together
Our Mission
We will deliver a quality patient experience in an academic health care environment that is responsive to the needs of the population of Northwestern Ontario.
Our Philosophy
Patient and Family Centred Care is the philosophy that guides us. Patients and Families are at the centre of everything we do.
We will focus our efforts on Patient Experience, Seniors' Health, Comprehensive Clinical Care, Aboriginal Health and Acute Mental Health.
Our Values
Patients ARE First:
Patients and families at the centre of everything we do. At our acute health care facility, we provide care to the people of Northwestern Ontario - a region the size of France.
Ours is the teaching hospital of choice for over 1,500 learners from the Northern Ontario School of Medicine, Lakehead University, Confederation College, and other partnering academic institutions. We are an academic health sciences centre, committed to teaching the next generation of health care providers and advancing medical research. Patients benefit from interprofessional teams of healthcare providers and access to leading-edge medical equipment and clinical trials.
Providing effective health care for patients and families has earned us both Innovation Awards and Leading Practice Designations. We are a national leader in Patient and Family Centred Care.
The Health Sciences Centre belongs to the community it serves; the 250,000 residents of Northwestern Ontario. Our Strategic Plan 2020 was built by and for them.
We are pleased to provide this report on the 2017-2018 fiscal year progress of the Strategic Plan 2020.
Leader Messages
Message from the Chair of the Board of Directors

Our Hospital board is accountable for the quality performance of the Hospital and provides oversight on decisions. Like many other health care boards in Canada, until recently, our board focused more on financial performance than clinical quality and patient safety. Recognizing the need to focus equally on quality, the board of directors invited Dr. Ross Baker, renowned author, professor, and researcher on Quality and Patient Safety to our annual retreat. We welcomed the opportunity to learn how to lead the organization to make improvements in quality of care and patient safety.
There is strong evidence to show that hospitals achieve excellent results when boards spend time engaging and challenging management on the quality of care improvement strategies. Key steps for the board include working with administration to identify ways for measuring quality of care and supporting our Hospital leaders to foster a culture of quality and safety. The board is very engaged and is fortunate to have a complement of diverse skill sets and experience. The Board regularly reviews and revises the board skill requirements and recruits to ensure the board has the required skills to lead the Hospital in improving quality and patient safety and other system priorities on the horizon.
Improving quality of care and patient safety is not a one-year project; systemic changes like this take time. Already, the Hospital has developed a Quality Health Care Framework which will help assess the care provided against six evidence-based criteria. The framework takes our Patient and Family Centred Care philosophy a step further by involving all people in the health care continuum: patients, families, staff, leaders, administration, partners, and the board. The board is confident that the implementation of the framework will result in significant changes to our Hospital’s quality culture and improvements to quality and patient safety.
On behalf of the Board of Directors, my congratulations is extended to the many leaders, staff, physicians and patients who contributed to the development of the Quality Health Care Framework, and for the many other important strategic achievements realized in 2017/18.
As this is my last Annual Report as Chair of the Board, I take this opportunity to express my gratitude to the many people who have provided guidance, support and incredibly hard work during my terms. Thank you to all the board members this year for your dedication and service. I have every confidence that our board members and leadership team will continue to implement the Strategic Plan 2020 successfully. We are Healthy Together.
Thank you.
Nadine Doucette
Chair, Board of Directors
Message from the President and CEO

Continuously improving safety and quality of patient care is a primary goal at the Thunder Bay Regional Health Sciences Centre. It falls under “Patient Experience”, one of five directions in our Strategic Plan 2020. We have developed, implemented and followed the Patient and Family Centred Care (PFCC) philosophy for over 10 years now, which has fostered improved patient experiences. This past year, our focus has been to extend PFCC to improve and measure the quality of care we provide.
This fairly straightforward goal can be deceptively difficult because “quality of care” is multidimensional, making it harder to measure. Indeed, patients may define quality of care differently from the staff providing the care. We developed the Quality Health Care Framework called STEEEP designed to both define quality of care and give us a way to measure it. STEEEP is an acronym of the six criteria that characterize quality of care: Safe, Timely, Effective, Efficient, Equitable, and Patient and Family Centred. In other words, if a program or service meets these six criteria, we can be more assured that our Hospital is providing quality patient care in that area.
Defining quality of care in this way was an important first step. To assist our professionals in ensuring we provide the most current care, we also introduced Quality-Based Procedures (QBP) Patient Digital Order Sets that standardize procedures to the point that we can accurately measure quality patient care and even compare our performance against other hospitals across Ontario. Our clinical teams have been involved in finding how these best practice order sets can be applied to their programs and services. This will be a fairly long process with key quality initiatives being identified and acted upon over the next five years.
Some programs have seen positive actions already. In September 2017, the Hospital introduced five provincial QBP Patient Digital Order Sets focused on six key Quality Improvement Plan (QIP) indicators: chronic obstructive pulmonary disease (COPD), chronic heart failure (CHF) in addition to pneumonia, hip fracture, hip replacement, and knee replacement. These standardized procedures can all be linked to quality of care indicators such as completion of the Patient Digital Order Sets within established provincial timelines, length of stay, re-admission rates, and others.
The results so far have been encouraging: within the first three months, 650 order sets in the six QBPs were used representing 81% of the patients treated during that time. They were used by surgeons 100% of the time, while uptake by medical specialists rated at 44%. Our goal is to increase the latter number to 100% across the board, and to roll out order sets for more QBPs.
We can’t complete such an ambitious project without the dedication of all staff at the Thunder Bay Regional Health Sciences Centre including our medical leaders and professionals. I am impressed with the progress our staff has demonstrated so far. The framework now in place will foster continuous improvement of the quality of care we provide our patients.
Many other successes were realized in 2017/18, and I encourage you to learn about them in this report. All areas of the Strategic Plan 2020 were advanced, and we are on track to meet our commitments. This is possible due to the outstanding commitment of our staff, physicians, researchers, Patient Family Advisors, volunteers, partners and donors. I am grateful to you all.
Thank you.
Jean Bartkowiak

President & CEO
Message from the Co-Chair, Patient and Family Advisory Council

Thunder Bay Regional Health Sciences Center continues to be a leader in the way we integrate the patient voice into everything that we do. Patient and Family Centred Care (PFCC) is our guiding philosophy, and it ensures that patients are true partners in their health care journey.
Our Hospital has been recognized and celebrated provincially, nationally and even internationally for our PFCC philosophy. It has improved the way we deliver health care and has made patients and families across Northwestern Ontario feel more connected to our Hospital. After all, we are all in this together.
One of the key components of our PFCC philosophy is the delivery of safe and quality care that results in a positive patient experience. We define the patient experience as the “whole” of your visit from the time you walk through our doors until you’re discharged. Under our Strategic Plan 2020, we have been putting extra focus on how we can improve the quality of care that we deliver and making sure we do it in the safest way possible.
Our strategic plan was designed so that PFCC would be the thread that held our programs and services together, along with corporate initiatives that focus on improving quality of care. As a Patient and Family Advisor (PFA), I am proud of how patients are becoming more involved in health care delivery. I’m also proud of the Hospital staff and administration for making quality and safety the focus of their work – it’s how we become healthy together.
Thank you.

Co-Chair, Patient and Family Advisory Council
Message from the Medical Advisory Committee

2017/18 has been a demanding year for our health care teams, though the challenges we faced are not unique to Thunder Bay. They are part of a provincial trend that will require system-wide assessment and system-wide solutions.
Challenges aside, the Medical Advisory Committee (MAC) has made significant advances in patient care at Thunder Bay Regional Health Sciences Centre. We are developing strategies to improve efficient care and to reduce unnecessary delays to improve patient flow and reduce length of stay (LOS). Quality, safety, and our Patients First approach continue to be the primary objectives of all frontline staff, including the professional staff. We have embraced the Kaizen strategy for continuous improvement, which has enabled us to focus on quality and safety as we launch new programs.
Medical Assistance in Dying (MAiD) is one of those new programs. We are lucky to have a capable, passionate team led by Dr. Andrew Turner, Dr. Margaret Woods, and Cathy Covino. This initiative moved forward with the help of feedback from key stakeholders including St. Joseph’s Care Group, North West Community Care Access Centre, and regional organizations including the Professional Staff Association (PSA). Death with dignity is our core philosophy, and the result has been significant quality and safety improvements for patients receiving end-of-life care. Information received from the MAiD Debriefing Sessions indicates this has been a significant quality improvement for our patients.
We are also moving towards a new Quality Improvement Plan (QIP) initiative that will make tracking and quantifying our progress easier. In September 2017, the Hospital introduced the first five Quality Based Procedure (QBP) Order Sets: chronic obstructive pulmonary disorder, congestive heart failure, pneumonia, hip fracture, and hip and knee replacement. These approaches, developed by Health Quality Ontario (HQO), will help standardize patient care and quality indicators. Hospital staff is also working with the North West LHIN, the Ministry of Health and Long-Term Care, and Think Research to develop an Opioid Order Set. The Hospital and the Lake of the Woods District Hospital in Kenora will be the two beta testing sites in the North West LHIN.
Professional staff leadership and engagement remain top priorities for the Chief of Staff with the goal of building leadership from within. This entails providing coaching, mentorship, and inspiration to younger professional staff to help them develop leadership skills. Learning is based on the Hospital administration’s “Me to We to All” leadership model. Engagement plays an important role, improving quality and safety, the patient experience, and clinician satisfaction. A survey sent out to the professional staff in spring 2018 will inform us where we need to focus in the coming year.
I would like to thank an incredible team of loyal and dedicated professional staff for their unyielding commitment to deliver care that is entrenched in our STEEEP (Safe Timely Efficient Effective Equitable Patient and Family Centred) quality framework. Despite the health care challenges we faced this year, we have maintained our focus to deliver on our Mission, uphold our Values, and succeed in our Vision to be “Healthy Together”.
Thank you
Dr. Gordon Porter

Chief of Staff
Chair, Medical Advisory Committee
Patient Experience
We are leaders in Patient and Family Centred Care (PFCC), and it is the philosophy that guides us. We recognize that creating a quality patient experience builds upon this philosophy.
We are focused on enhancing the Patient Experience as one of our strategic priorities. Our goals are to:
- Develop a framework to deliver high quality care;
- Enhance understanding and continue to grow and embed our PFCC philosophy;
- Advance the academic environment;
- Invest in staff development, engagement and wellness;
- Use information technology to advance the patient experience.
We will know we are successful by 2020 when we demonstrate:
- No harmful events;
- Patients are highly satisfied & engaged in care;
- A research culture;
- Learners are satisfied;
- Staff and physicians are engaged in care;
- Advanced information technology supports patients and care providers.
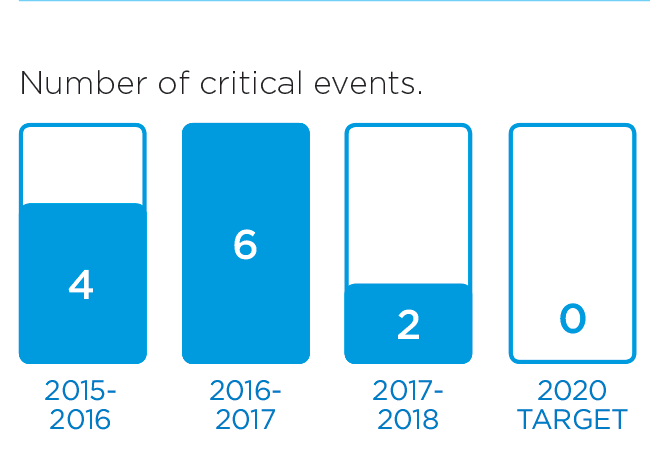
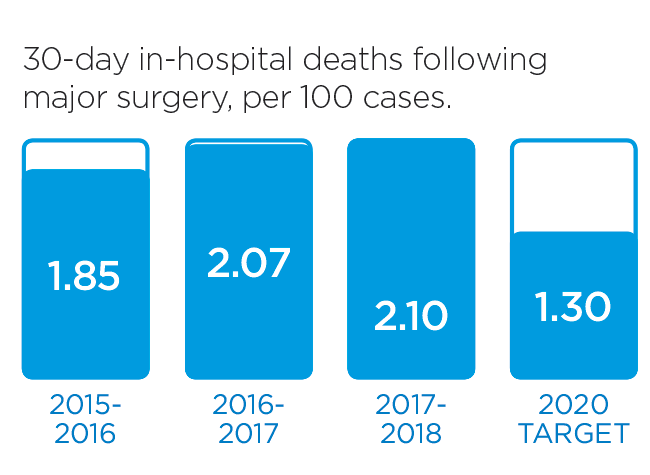
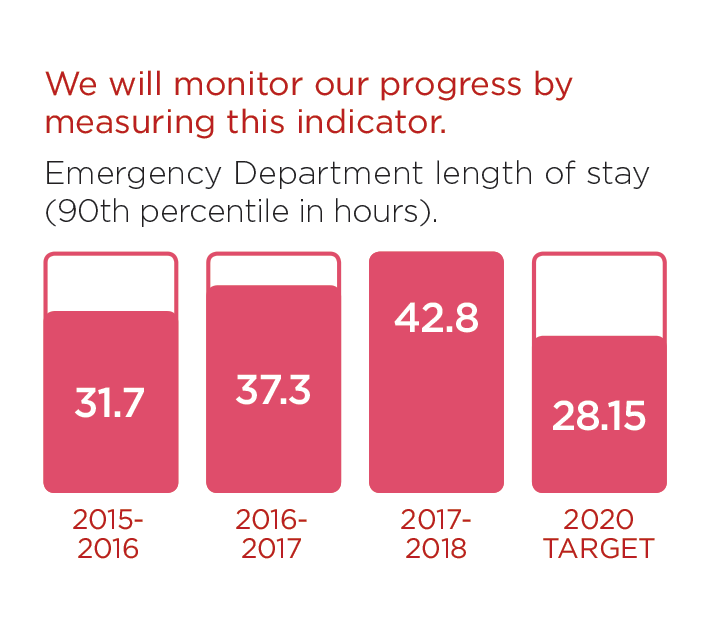
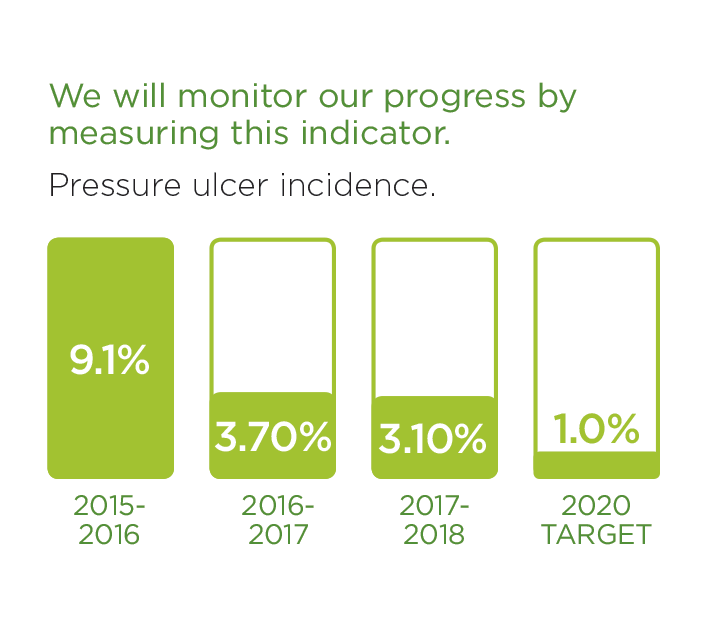
We will monitor our progress by measuring these indicators.

These stories provide an insight into three of the many Patient Experience initiatives in 2016/17:
Improving Patient Experiences in the Emergency Department
Thunder Bay Regional Health Sciences Centre has one of the busiest Emergency Departments in Ontario with about 9,000 visits per month. With so many patients coming through on a daily basis, the Emergency Department (ED) team is committed to ensuring that each one is satisfied with the care they receive.
Leading with Respect
Promoting a positive and respectful environment begins with positive and respectful leaders. Thunder Bay Regional Health Sciences Centre is applying that approach to continued leadership development and enhancement training, which will ultimately improve patient experiences.
Improving Patient Experiences in the Emergency Department
Thunder Bay Regional Health Sciences Centre has one of the busiest Emergency Departments in Ontario with about 9,000 visits per month. With so many patients coming through on a daily basis, the Emergency Department (ED) team is committed to ensuring that each one is satisfied with the care they receive.
“We’re always looking for ways to improve patient satisfaction and the overall patient experience,” said Lisa Beck, Director of the Trauma Program, Critical Care and Emergency Services. “Since patients are at the centre of everything we do, the best way for us to improve is to ask our patients directly how we can do better. Their feedback is applied to Patient Experience Action Plan, where we adapt our services to meet the needs identified.”
One way our Hospital gathers meaningful input from ED patients is through National Research Corporation (NRC) patient satisfaction surveys that are offered to all ED patients. The results are reviewed on a monthly basis so that Hospital administrators can evaluate the impact of changes we’ve implemented.
“Not all ED patients fill out the survey, so we also gather input through a Patient and Family Advisor who actually engages with patients while they’re in our Emergency Department,” said Beck. “We’ve found that real-time feedback to be really helpful and a great example of our Patient and Family Centred Care philosophy at work.”
A common theme among patient feedback was the desire for more information on how the ED works and what can be expected. Patients wanted to know how it’s determined which ED patients are seen first, about visitor policies, and other patient guidelines and policies.
“We understand that visits to the ED can be very stressful and we want to ease the anxieties of our patients and their families,” said Tyler Van Ramshorst, Operations Coordinator for Emergency and Trauma Services. “We now provide a brochure that explains everything ED patients need and want to know while they’re here for care.”
Since the Patient Experience Action Plan has been implemented, ED patient satisfaction rates have improved by 23%, rising from a starting point of approximately 57% to 70% in all dimensions.
“Our improvement efforts are ongoing, but we’re really proud of the progress we’ve made so far,” said Van Ramshorst. “Everyone involved in the working group, and our nurses in particular, have fully embraced the plan and are completely engaged and committed to patient satisfaction. The level of professionalism and dedication to Patient and Family Centred Care under what can be very challenging circumstances is really remarkable. We’re fortunate to have such caring staff in our Emergency Department.”

Thunder Bay Regional Health Sciences Centre’s Emergency Department team is committed to ensuring that all patients are satisfied with the care they receive.
Leading with Respect
Leadership at Thunder Bay Regional Health Sciences Centre is undergoing development and enhancement training to help support a more respectful environment, ultimately improving patient care.
Promoting a positive and respectful environment begins with positive and respectful leaders. Thunder Bay Regional Health Sciences Centre is applying that approach to continued leadership development and enhancement training.
This new approach to leadership training builds upon the “Me to We to All” method launched last year. It builds upon each leader’s individual strengths to create more collaborative and supportive teams, and ultimately improve patient care.
“Our goal is to increase the knowledge and competency of staff in the areas of acute mental health, senior’s health, Indigenous health and culture, accessibility and the patient experience overall,” said Amanda Bjorn, Executive Vice President of People, Culture and Strategy. “The training is designed to build skills and knowledge to support a respectful environment. In the end, we want all staff to be considerate and kind towards everyone – coworkers, patients and families – and to acknowledge everyone else’s experiences, views and beliefs.”
Hospital employees, volunteers and professional staff will participate in respect education training, which is being lead by the Hospital’s Interprofessional Education department. The training will be delivered through an innovative mixed methodology approach to learning that includes self-assessments, e-learning, in-situ simulation activities, and coaching. A key factor of this education is that all leaders are to be trained as coaches and will take on a key role throughout implementation. The majority of education will provide opportunities for participants to practice techniques and skills and to have meaningful interactions regarding content. Finally, a support component has been built into the training plan to facilitate behaviour and culture change.
“Respect isn’t something that can be taught in a classroom, it’s something that begins within each individual person through self reflection,” said Bjorn. “Everyone should be treated with respect, regardless of age, illness or culture, and accomplishing that starts with ourselves. This approach to learning will help people to understand their own biases and beliefs and how those biases impact others. This training will encourage introspective conversations that will explore thoughts and feelings in the work place, with a focus on racism and other stereotypes that can create barriers to optimal health care. Ultimately, we hope to create a safer space for everyone that comes to our Hospital.”

Leadership at Thunder Bay Regional Health Sciences Centre is undergoing development and enhancement training to help support a more respectful environment, ultimately improving patient care.
Comprehensive Clinical Care
We aim to enhance the Comprehensive Clinical Care that transcends the organization and touches all patients. Our activities are focused on addressing gaps in care, so the people of Northwestern Ontario can receive quality care, closer to home.We aim to enhance the Comprehensive Clinical Care that transcends the organization and touches all patients. Our activities are focused on addressing gaps in care, so the people of Northwestern Ontario can receive quality care, closer to home.
Within Comprehensive Clinical Care, we have identified the following Goals:
- Adopt the Ontario Chronic Disease Prevention and Management framework;
- Deliver comprehensive cardiovascular care in accordance with the Ministry of Health;
- Enhance access to clinical services supported by patient flow efficiencies;
- Develop formal partnerships to deliver comprehensive clinical services that support care in the appropriate location;
- Deliver a comprehensive acute pain management service.
We will know we are successful by 2020 when we demonstrate:
- Patients with chronic illness possess self-management skills;
- Access to comprehensive cardiovascular care service in NWO;
- Patient access, length of stay, admission and discharge process improved;
- Partnerships support care closer to home;
- Access to comprehensive acute & chronic pain management.
Learn more about our exciting progress in this area:
Hospital Welcomes Second Vascular Surgeon
Thunder Bay Regional Health Sciences Centre is another step closer to offering a full cardiovascular program. In January, Dr. Elrasheed Osman joined our team of talented physicians. He is the second vascular surgeon at our Hospital, and key to our commitment to deliver comprehensive cardiovascular care.
Improving Patient Flow
Hospitals across Ontario are facing capacity challenges. Thunder Bay Regional Health Sciences Centre is no exception and has experienced uncharacteristically high patient admissions since the winter of 2017/18. In the face of ongoing capacity challenges, patient flow is a priority and ensures our patients receive the right care, at the right time, by the right provider.
Making Room for Hospital’s New Cardiovascular Surgical Program
A full cardiovascular surgical program at Thunder Bay Regional Health Sciences Centre is expected to be up and running in 2020. The burden of cardiovascular disease in Northwestern Ontario is well above the provincial average. Meeting the acute care needs of our patients means providing cardiac and vascular care close to home. Capital planning is now underway, bringing our Hospital one step closer to launching the new program.
Hospital Welcomes Second Vascular Surgeon
Thunder Bay Regional Health Sciences Centre is another step closer to offering a full cardiovascular program. In January, Dr. Elrasheed Osman joined our team of talented physicians. He is the second vascular surgeon at our Hospital, and key to our commitment to deliver comprehensive cardiovascular care.
The addition of Dr. Osman and his knowledge and experience improves our capacity to provide much needed vascular services, closer to home, for patients across Northwestern Ontario. Dr. Osman joins our other vascular surgeon, Dr. Mary MacDonald, who joined our team in October of 2016.
With two highly skilled vascular surgeons, we can provide life-and-limb saving care in a much more timely fashion. This means patients across Northwestern Ontario will have shorter wait times for treatments, closer to home. Previously, patients would have had to travel to Southern Ontario, resulting in heightened levels of stress and additional financial burdens.
For critical and emergency patients in particular, local access to vascular surgery can make all the difference in terms of saving lives and limbs, which is particularly important for our patients and families since amputations occur more frequently in Northwestern Ontario than the rest of the province. With two surgeons now in place, we hope to improve vascular health in the Northwest by making arterial bypass surgery more accessible.
Last year, Dr. MacDonald dealt with approximately 245 vascular cases. With the arrival of Dr. Osman, we can double the number of patients who will benefit from their services. By the end of the year, we will welcome a third surgeon to our team, enabling us to handle over 600 vascular procedures annually.

Dr. Mary MacDonald and Dr. Elrasheed Osman are helping bring much needed vascular services, closer to home, for patients across Northern Ontario.
Improving Patient Flow
Hospitals across Ontario are facing capacity challenges. Thunder Bay Regional Health Sciences Centre is no exception and has experienced uncharacteristically high patient admissions since the winter of 2017/18.
In the face of ongoing capacity challenges, patient flow is a priority and ensures our patients receive the right care, at the right time, by the right provider. Patient flow refers to the way care is planned and delivered, including medical care, physical resources, and internal systems. In other words, patient flow refers to the care and resources needed to support patients throughout their journey at the Hospital, from admission to discharge and beyond, while maintaining safety, quality and patient satisfaction.
“Patient flow remains as one of the largest issues affecting our Hospital, especially when you factor in that our Emergency Department (ED) is one of the busiest in the province. Of all the people who come to our ED, many need to be admitted,” said Dr. Stewart Kennedy, Executive Vice President of Medical, Academics, and Regional Programs. “Every improvement means that an admitted patient in the ED can move into an inpatient bed sooner.”
A large contributing factor to patient flow and overcapacity is Alternate Level of Care (ALC) patients who no longer need to be in a hospital, but still require some form of health care such as rehabilitation, home care, or a long-term care facility. Unfortunately, the needs for such services often exceed what our community agencies can provide.
“By focusing on how and when we admit and discharge patients, and finding efficiencies in processes, we have reduced the amount of time patients spend waiting in the Hospital when they don’t need to. Efficiency means getting patients well sooner,” said Dr. Kennedy.
An example is the introduction of an electronic system used at the bedside by clinicians. The information in the system allows members of the health care team to see and address potential delays in services for patients, such as diagnostic testing or physiotherapy.
Working together with health system partners is also important to ensure that patients receive safe, quality care. “We are all committed to enhancing the coordination of care to support best possible outcomes and experiences for patients and work closely on a daily basis,” explained Kennedy.

Dr. Stewart Kennedy, Executive Vice President of Medical, Academics and Regional Programs at Thunder Bay Regional Health Sciences Centre
Making Room for Hospital’s New Cardiovascular Surgical Program
A full cardiovascular surgical program at Thunder Bay Regional Health Sciences Centre is expected to be up and running in 2020. The burden of cardiovascular disease in Northwestern Ontario is well above the provincial average. Meeting the acute care needs of our patients means providing cardiac and vascular care close to home. Capital planning is now underway, bringing our Hospital one step closer to launching the new program.
“We are excited to be making significant progress, in collaboration with the University Health Network’s Peter Munk Cardiac Centre,” said Arlene Thomson, Senior Director, Cardiovascular Program Development and Implementation. “We are working closely with the Capital Planning Branch at the Ministry of Health and Long-Term Care to ensure our facility is ready to offer these new, much needed services.”
The new program will require more beds, specifically for cardiovascular patients. Our Hospital is also working with architects and planners to identify appropriate locations for the new areas that will be needed for this program. This includes 19 additional patient beds, a new surgical suite and related renovations, new vascular lab, renovations to Ambulatory Care and Central Processing and other updates as required.
“Right now, our goal is to build within our Hospital walls where possible. An expansion of our current Hospital is likely, and will be done within accordance of Ministry guidelines and in such a way that will support our ability to provide quality patient care across all clinical units.”
The Ministry of Health and Long-Term Care has committed to funding 90% of the construction costs associated with the project. It will be up to our community to cover the remaining 10% of the construction costs plus 100% of the capital equipment costs.
To learn more about cardiovascular care at our Hospital, please visit http://tbrhsc.net.

Arlene Thompson, Senior Director of Cardiovascular Program Development and Implementation, looks over expansion plans for the Hospital’s new Cardiovascular Surgical Program.
Seniors' Health
The population of seniors is growing. Baby boomers' health care needs will continue to increase. We recognize that the care needs of seniors are different, and will tailor services to accommodate them.
To advance care for the aging population, we will focus on these Goals within Seniors' Health:
- Deliver an optimal experience for seniors;
- Adopt the Ontario Senior Friendly Hospital Framework.
We will know we are successful by 2020 when we demonstrate:
- Seniors' hospital experience is optimal;
- Seniors and their families are highly satisfied and engaged in care.
We have made progress in this area already. These stories are examples of initiatives that are underway.
Early Interventions Improve Care for At-Risk Seniors
Service demand is growing for senior patients. In addition to requiring health care more often, their needs are different from the general population. Thunder Bay Regional Health Sciences Centre has implemented a new program to ensure that senior patients are receiving the right care, at the right time, and by the right provider.
Lose the Tube: Hospital Adopts New Medical Directive to Improve Seniors’ Health
Over-use of urinary catheters has been a common trend in Hospitals, and one that particularly affects senior patients. Thunder Bay Regional Health Sciences Centre is committed to improving seniors’ health and has pledged to “lose the tube”; an initiative that will improve patient care by reducing the length of time a urinary catheter is in use.
A patient may require a urinary catheter for a variety of reasons. A new medical directive empowers nurses to remove the catheter when it is no longer needed, which can reduce incidences of urinary tract infections.
Over-use of urinary catheters has been a common trend in Hospitals, and one that particularly affects senior patients. Thunder Bay Regional Health Sciences Centre is committed to improving seniors’ health and has pledged to “lose the tube”; an initiative that will improve patient care by reducing the length of time a urinary catheter is in use.
What is a medical directive?
Medical directives are written orders to perform treatments or procedures on patients when specific conditions are met.
“Research has shown that patients greatly benefit from early removal of unnecessary catheters. It not only reduces the risks of infection, but also enables patients to be mobilized much sooner,” said George Fieber, Nursing Practice Lead. “This new medical directive, introduced and championed by Dr. Zaki Ahmed and Dr. Margaret Woods, empowers nurses to make an informed judgment call about how soon catheters can be safely removed.”
The new process was based on a toolkit developed by Choosing Wisely Canada in association with the Canadian Society of Internal Medicine. It supports physicians and nurses in three areas of focus:
- Early removal of unnecessary urinary catheters on inpatient wards
- Restrictive insertion of urinary catheters in operating rooms
- Restrictive insertion of urinary catheters in emergency departments
“We’re building on the best practices and directives provided by the toolkit in order to better address the needs of our Hospital, and the patient population that we serve,” said Fieber. “This is a great initiative that will help improve the experiences of our senior patients and is reflective of our Patient and Family Centred Care philosophy.”

Andrea Raynak, Clinical Nurse Specialist, Chronic Disease Prevention and Management.
Early Interventions Improve Care for At-Risk Seniors
Service demand is growing for senior patients. In addition to requiring health care more often, their needs are different from the general population. A new program at Thunder Bay Regional Health Sciences Centre supports senior patients to receive the right care, at the right time, and by the right provider.
"My family recently experienced the Hospital's Geriatric Program when our Step-Dad was diagnosed with dementia. He was assessed early in his admission to the Emergency Department and was monitored closely throughout his stay by the Geriatric Care Coordinator,” said a family member. “We had been struggling at home with his changing care needs but the team listened to us and guided his care accordingly, keeping us informed every step of the way. We're very impressed by the level of care our Dad received and are hopeful, that as a result, he can remain healthier and at home."
Beginning in the Emergency Department, the Program aims to streamline the assessment process of at-risk seniors through collaboration with internal and external partners, consultation with geriatricians, physicians, St. Joseph’s Care Group, and the North West LHIN’s Home and Community Care.
“When at-risk or frail senior patients aged 65 years and older arrive at our Hospital, they are assessed using standardized tools. A Geriatric Care Coordinator can identify potential geriatric health concerns and facilitate the appropriate care plan,” said Ron Turner, Senior Director of Patient Care and Health Professions. “By providing senior friendly care early, we can achieve improved continuity of care, enhanced patient experiences and better outcomes.”
During assessment, the Geriatric Care Coordinator looks for signs of geriatric syndromes, including mobility issues, weakness, frailty, functional decline, pain, cognitive impairment, dementia, delirium, and other risk factors often associated with seniors. The Geriatric Care Coordinator also supports discharges for patients who do not require acute care in a hospital setting; and works with community partners to provide a smooth transition to home or other programs and services that would best address their needs.
“Research has shown that prolonged hospital stays can lead to further complications, particularly for senior patients,” said Turner. “Having someone on the team who is directly responsible for organizing their care needs ensures that patients will get the appropriate level of care they need, in a safe way and without undo delays.”
So far, the program has yielded successful results. The average length of stay for senior patients has decreased and continues to do so as the program progresses. Patient experiences have been enhanced and families and caregivers have expressed content with their level of inclusion in the care plans of their loved one and the ongoing support provided after discharge.
To learn more about our Hospital’s commitment to seniors’ health, visit www.tbrhsc.net.

A new Geriatric Program at Thunder Bay Regional Health Sciences Centre provides early assessment and interventions to ensure senior patients receive the right care, at the right time, and by the right provider.
Indigenous Health
Enhance culturally appropriate care.
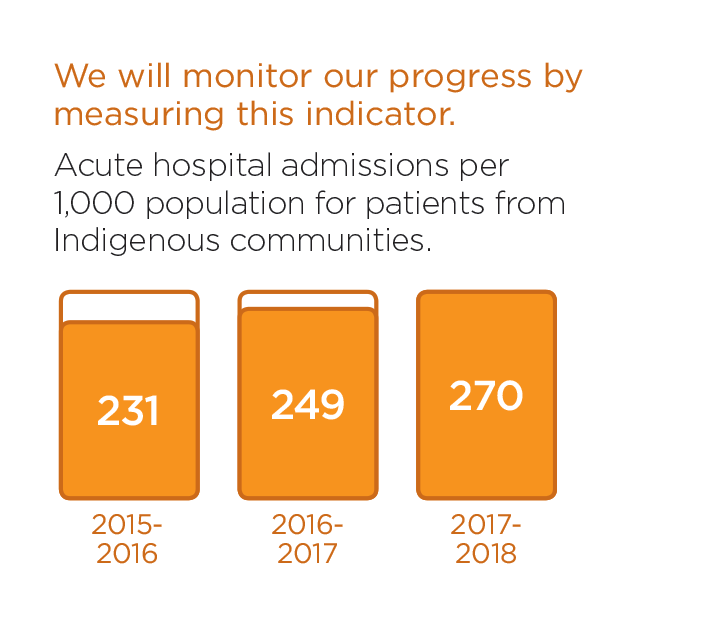
Indigenous people, particularly those from remote communities, face unique challenges to access to health care. In addition to geographical, language and cultural barriers, there are socioeconomic realities that simply do not exist outside of this population. Indigenous people account for at least 19% of our population. Unfortunately, they are the least healthy people in our region.
We aim to improve experiences and outcomes for Indigenous patients and families by providing care that is culturally relevant and sensitive, in welcoming environment.
Our Indigenous Health Goals are:
- Provide care that improves self-management, access, experience, and transition to home for Indigenous patients;
- Provide health care that respects traditional knowledge and practices, and builds TBRHSC as a leader in the provision of health care for Indigenous patients.
We will know we are successful by 2020 when we demonstrate:
- Indigenous patients from remote communities equally access, self-manage and transition to home;
- Indigenous people feel welcomed.
Please read about recent activities in this area.
Enhancing Indigenous Health Through Partnership
Indigenous people in our community are sicker than non-Indigenous people. One reason for this is access to culturally safe primary care. Stronger links between primary care (family physicians, nurse practitioners) and acute care (hospital) can help. That’s why Anishnawbe Mushkiki Community Health and Wellness and Thunder Bay Regional Health Sciences Centre are working together.
Protocol Protects Children
To provide the best level of care and support to patients, hospitals work in collaboration with many other service providers. Each patient has different needs, and may already be receiving service from another organization. Thunder Bay Regional Health Sciences Centre and Dilico Anishinabek Family Care recently signed a new agreement that ensures coordination of care for children and families who require or are already receiving Child Welfare Services.
Enhancing Indigenous Health Through Partnership
Indigenous people in our community are sicker than non-Indigenous people. One reason for this is access to culturally safe primary care. Stronger links between primary care (family physicians, nurse practitioners) and acute care (hospital) can help. That’s why Anishnawbe Mushkiki Community Health and Wellness and Thunder Bay Regional Health Sciences Centre are working together.
“We initially met to better understand each other’s role in the community, and quickly realized the potential to enhance care and experiences for Indigenous patients,” said Jean Bartkowiak, Hospital President & CEO.
Anishnawbe Mushkiki Executive Director Michael Hardy was immediately encouraged by the opportunity. “We can be even more responsive to Indigenous needs, values and preferences,” he said. “We can break down the silos between health care sectors and providers to ensure seamless transitions for patients. We will truly be working together to provide patient and family centred care across the continuum of care.”
Anishnawbe Mushkiki is an Indigenous-led Primary Health Care Organization. Their health care team includes physicians, nurse practitioners, nurses including footcare and wound care specialist, dietitians, diabetes educators, social workers, traditional healers and other health care professionals.
At Anishnawbe Mushkiki, clients can access a variety of services, including clinical care and integrated chronic disease prevention and management, family-focused maternal and child health care, addictions counselling, traditional healing, counselling, youth empowerment and cultural programs.
Working more closely together can address current disparities affecting the urban Indigenous population in Thunder Bay. For example, some patients who visit the Hospital Emergency Department (ED) could be seen in a primary care setting. On discharge, the Hospital can refer such patients to Anishnawbe Mushkiki , where they can be connected to a family physician or nurse practitioner for ongoing care. “Patients would benefit from continuity of care and wellness programs to improve overall health,” explained Hardy.
There are benefits to the health care system, too. “By improving overall health, future ED visits are prevented,” noted Bartkowiak. “Thousands of visits to the ED could be diverted, which translates to improved wait times and resource utilization for those requiring acute care services at our Hospital.”
The collaborative approach goes beyond the Emergency Department. “Our organizations are exploring and moving forward with initiatives that enhance access to other areas of care. One is transition services from in-patient to out-patient for Indigenous mental health patients,” said Hardy.
It all aligns perfectly with Anishnawbe Mushkiki’s mission to provide culturally safe, comprehensive care empowering patients through their health and wellness journeys by offering health promotion, primary and traditional approaches to patient and family centred care, and with the Hospital’s commitment to Indigenous Health.

Michael Hardy, Executive Director of Anishnawbe Mushkiki and Hospital Board Director, and Jean Bartkowiak, Hospital President & CEO are working together to improve the health of Indigenous patients and families.
Protocol Protects Children
To provide the best level of care and support to patients, hospitals work in collaboration with many other service providers. Each patient has different needs, and may already be receiving service from another organization. Thunder Bay Regional Health Sciences Centre and Dilico Anishinabek Family Care recently signed a new agreement that ensures coordination of care for children and families who require or are already receiving Child Welfare Services.
“We value our relationship with Dilico,” explained Ron Turner, Senior Director of Patient Care and Health Professionsat the Hospital. “The service protocol supports us both to provide the most appropriate care."
The child welfare services protocol identifies standards for point of contact, methods of contact, and purpose of contact between the Hospital and Dilico to reduce trauma to children by improving coordination.
Darcia Borg, Dilico Executive Director, noted the protocol improves child abuse responses and supports families. "The protocol is effective because it defines the purpose and scope of coordination and collaboration, describes the roles and responsibilities of each organization, and outlines the steps to be completed at each stage. When everyone involved knows exactly what steps to take, the best interests of the child are protected," she said.
Dilico Anishinabek Family Care provides a range of responsive individual, family and community programs and services for the complete life journey of all Anishinabek people. Dilico cares for the welfare of children and families, physical health, the mental health and the health of the communities where Anishinabek people live by promoting wellness, preventing illness and trauma, and providing diagnosis, treatment and rehabilitation.

Darcia Borg, Dilico Executive Director, signs a new agreement with our Hospital that ensures coordination of care for children and families who require or are already receiving Child Welfare Services.
Acute Mental Health
Enhance acute mental health service.
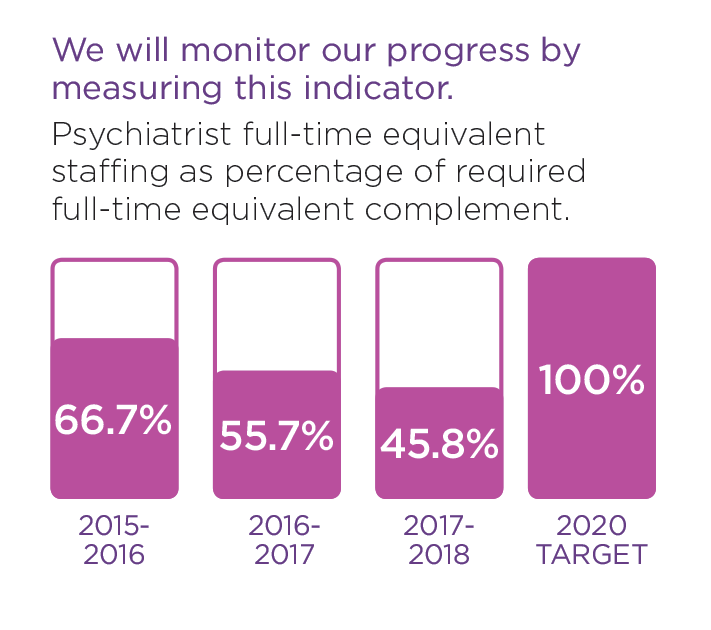
While Acute Mental Health inpatient days are decreasing at other hospitals, it has increased by 5.4% here. We want to be sensitive to patient needs, ensuring that mental health is viewed as part of overall health. We believe that everyone should be respected equally, regardless of age, illness or culture and will strive to provide a more holistic approach to treat the full human being – mind, body, and soul.
Within Acute Mental Health, we will:
- Adopt attitudes and behaviours that recognize mental health as an integral part of the delivery of comprehensive acute care services;
- Enhance the delivery of mental health care to patients outside of mental health services;
- Collaborate with system partners and appropriate governing agencies to develop and enhance transition in care;
- Enhance the delivery of acute mental health care within mental health services.
We will know we are successful by 2020 when we demonstrate:
- The hospital supports a stigma-free environment;
- Access to Psychiatry service.
These stories provide examples of our commitment in action.
Hospital Plans to Improve Mental Health Emergency Services
Northwestern Ontario experiences high rates of mental health concerns. Because of this, Thunder Bay Regional Health Sciences Centre is prioritizing Acute Mental Health with plans to significantly improve mental health emergency services. Planning is underway for a Mental Health Emergency Service (MHES) at the Hospital. The concept is to provide specialized care for patients who come to the Emergency Department in a mental health crisis, while also addressing the high demand for addiction services that exist within our community.
Consultation Liaison Service Improves Access to Mental Health Care
A new Consultation Liaison Service provides patients with referrals to psychiatric or behavioural management, liaison with the referring treatment team, ongoing monitoring of mental status, and facilitation of transfer to other mental health care services if deemed necessary. It is currently being piloted on Hospital units 1A and 2A.
Hospital Plans to Improve Mental Health Emergency Services
Northwestern Ontario experiences high rates of mental health concerns. Because of this, Thunder Bay Regional Health Sciences Centre is prioritizing Acute Mental Health with plans to significantly improve mental health emergency services.
Planning is underway for a Mental Health Emergency Service (MHES) at the Hospital. The concept is to provide specialized care for patients who come to the Emergency Department (ED) in a mental health crisis, while also addressing the high demand for addiction services that exist within our community. The MHES would provide a safe, secure and appropriate space for care and help reduce stigma and improve safety, privacy, comfort and ultimately the quality of care that our patients and their families receive.
“We see high volumes of patients in mental health crisis at our Hospital, which is likely due to a combination of socio-economic realities across our region,” said Dr. Peter Voros, Program Director, Adult and Forensic Mental Health. “We’ve really made mental health a priority in our Strategic Plan, ensuring that mental health is viewed as a crucial part of overall health. The development of a robust Mental Health Emergency Service located within our Emergency Department is an important step to improve care.”
The MHES will improve patient care and experiences by decreasing Emergency Department length of stay for patients presenting with mental health concerns. Under this new service, patients will be seen and assessed much sooner. The MHES is expected to help patients through the use of Psychiatric stabilization, thereby avoiding unnecessary admissions.
MHES will be staffed by an interdisciplinary team of professionals, including a physician, psychiatrist, nurses, social workers, administrative clerk and security. The service will require some expansion and renovations to our existing Emergency Department and other areas of the Hospital in order to ensure adequate space for the needs of our patients.
“Although the MHES is still in the early stages of development, we are confident it will help us better attend to the mental health status of our region,” said Voros. “Its benefits will not only improve the care and satisfaction of our patients and their families, but will also improve conditions for staff.”
To learn more about mental health services at our Hospital, visit http://tbrhsc.net/programs-services/mental-health-program/.

Dr. Peter Voros, Program Director of Adult and Forensic Mental Health, Thunder Bay Regional Health Sciences Centre.
Consultation Liaison Service Improves Access to Mental Health Care
Any patient could struggle with mental health. “It’s important that mental health is viewed as part of overall health and that we’re sensitive to the needs of our patients” explains Dr. Peter Voros, Program Director, Adult and Forensic Mental Health at Thunder Bay Regional Health Sciences Centre.
Patients with mental health concerns admitted to non-mental health units at our Hospital are now provided with increased access to specialized and appropriate mental health care they may need.
A new Consultation Liaison Service provides patients with referrals to psychiatric or behavioural management, liaison with the referring treatment team, ongoing monitoring of mental status, and facilitation of transfer to other mental health care services if deemed necessary. It is currently being piloted on Hospital units 1A and 2A.
“The service allows for a more robust assessment of patient needs by providing timely and efficient mental health care for adult patients admitted to medical, surgical and critical care units within our Hospital,” said Voros.
The liaison team consists of a mental health nurse and a psychiatrist. If a patient is displaying signs of psychological distress, then a member of their care team can request assistance from the consultation liaison. The mental health nurse will then meet with the patient to gather more information, provide care plan suggestions where appropriate, and help determine whether or not the psychiatrist is needed.
“Since the service has been up and running, patients are better cared for and receiving more robust assessment than before,” said Darcy Price, Manager of Adult Mental Health Services. “Patients who require the service are seen on a daily basis by the clinical liaison, which provides consistency for the patient and staff. Patients and families, and our staff now feel better supported.”
Based on the success of the Consultation Liaison Service pilot project, the Hospital aims to expand the service across the whole Hospital, ensuring all patients and their families are better cared for from a metal health perspective.

Dr. Hampe, a psychiatrist, and Nadia Bottoset, Case Manager with Adult Mental Health, are providing patients on non-mental health units of Thunder Bay Regional Health Sciences Centre with increased access to mental health care through the Consultation Liaison Service.
Vital Medical Equipment Funded Thanks To Donors
For patients requiring acute, specialized medical care, the Thunder Bay Regional Health Sciences Centre is the place to go in Northwestern Ontario. Thanks to donors, each year, the Hospital is able to continually update its medical equipment to provide this expert –level care. Because, just like technology evolves in our everyday lives, it does the same with healthcare equipment. The phone you had ten years ago is now almost unrecognizable. Similarly, medical equipment changes so rapidly that equipment from a decade ago can look entirely different today. Advances in medical equipment are fast and furious and donors provide the funding necessary to provide the latest generation of vital medical equipment. In fact, in 2017, your donations were responsible for providing $3,269,375 in funding which was distributed throughout the Thunder Bay Regional Health Sciences Centre.
In 2018, we are now on the cusp of a revolution of care in Northwestern Ontario as we prepare to welcome a full cardiovascular surgery program to Thunder Bay; a program that will provide both vascular and cardiac surgery to approximately 1,000 patients a year, who would otherwise have to travel to receive this life- and limb-saving care. It’s our time to work together to ensure our regional Hospital can offer this critical service.
For more information, including a full listing of grants made possible thanks to donors like you, visit: healthsciencesfoundation.ca/impact
Thunder Bay Regional Health Research Institute
Since our region is unique in its health care needs and challenges, it makes sense that our research program would be unique as well. The Thunder Bay Regional Health Research Institute promotes patient-centred research that focuses on finding interventions and other procedures to solve health care challenges most prevalent in Northwestern Ontario – intervetnions and other procedures that also have global applications.
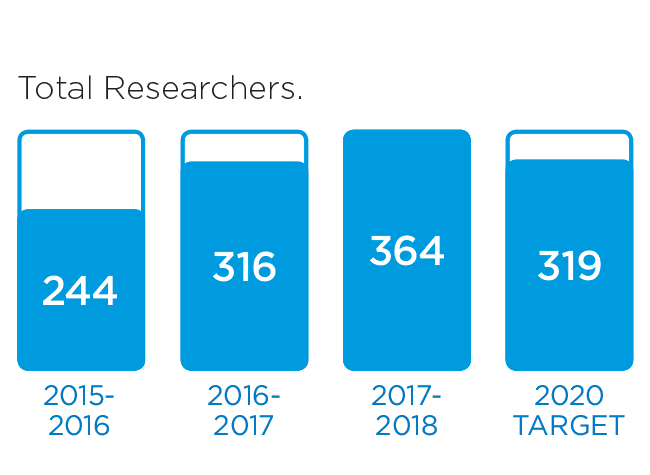
We encourage strong collaborations between our scientists and clinicians at the Thunder Bay Regional Health Sciences Centre and throughout the region to find homegrown solutions to the health care challenges that affect us most. The Health Research Institute follows the Council of Academic Hospitals of Ontario tenets of Healthier, Wealthier, and Smarter. Read more about it in our 2017/18 Annual Report.
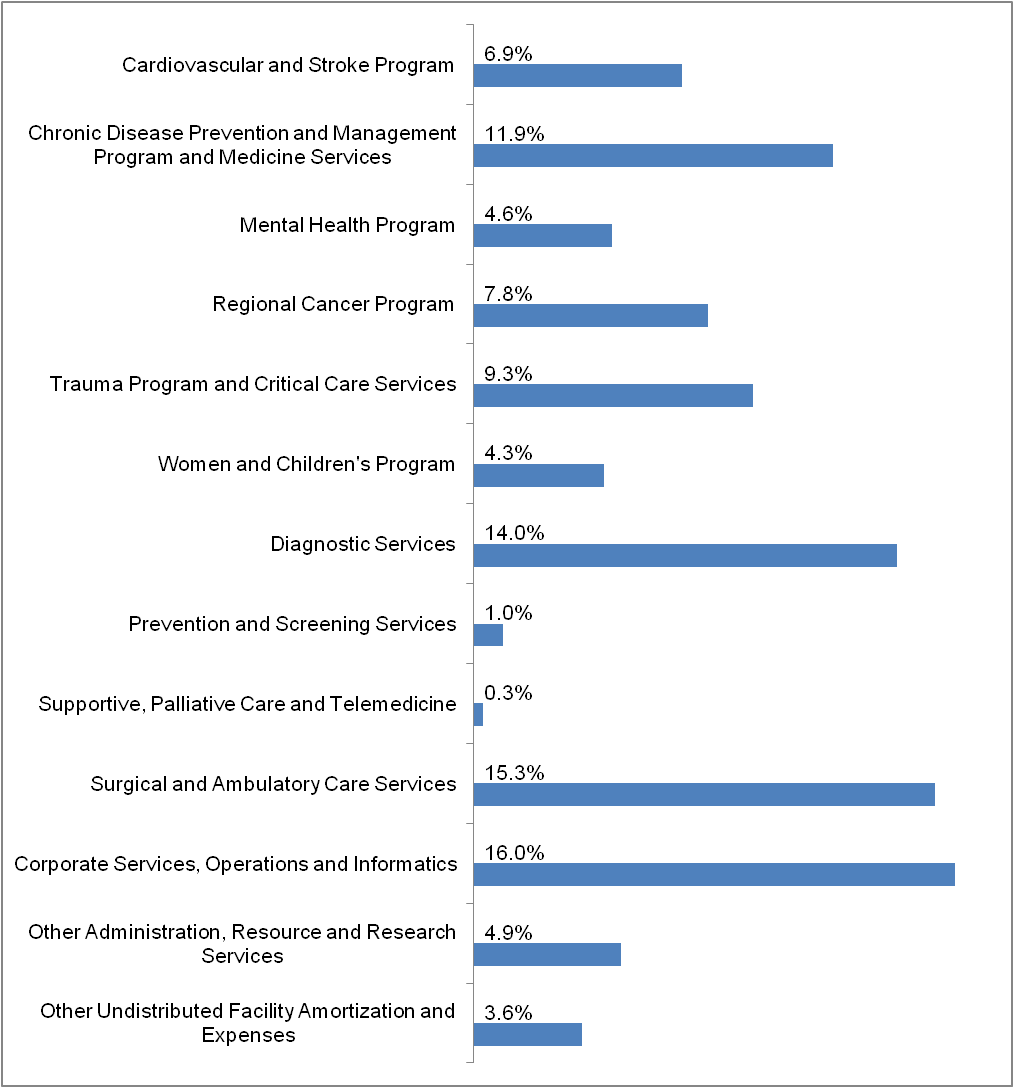
Financial Statements
Thunder Bay Regional Health Sciences Centre continues to manage health care resources effectively and responsibly, while providing quality acute health care for the residents of Northwestern Ontario. Our Health Sciences Centre continues to face service and financial pressures as a result of many fiscal, demographic and health care system challenges. In 2017/18, we regularly operated in surge capacity, and this creates significant financial pressures. Our budgeted deficit for 2017/18 was $5.9 million. In addition to measures we took internally, we received one-time funding from the North West Local Health Integration Network and the Ministry of Health and Long Term Care to address a majority of the deficit. We continue to work closely with the Local Health Integration Network and other community partners to address the ongoing challenges.
| FINANCIAL STATEMENTS | ||||||||
| STATEMENT OF FINANCIAL POSITION | ||||||||
| March 31, (Amounts in $ thousands) | 2018 | 2017 | 2016 | 2015 | 2014 | 2013 | 2012 | 2011 |
| Assets | ||||||||
| Current assets | 38,085 | 29,125 | 30,459 | 31,259 | 33,113 | 33,452 | 29,822 | 28,779 |
| Non-current assets | 228,829 | 241,497 | 252,981 | 272,029 | 260,039 | 238,660 | 246,473 | 256,185 |
| Total Assets | 266,914 | 270,622 | 283,440 | 303,288 | 293,152 | 272,112 | 276,295 | 284,964 |
| Liabilities and Fund Balances | ||||||||
| Current liabilities | 51,236 | 46,199 | 45,067 | 57,169 | 45,300 | 42,858 | 41,179 | 40,175 |
| Non-current liabilities | 207,088 | 219,330 | 234,449 | 240,113 | 236,634 | 218,603 | 227,040 | 233,508 |
| Total liabilities | 258,324 | 265,529 | 279,516 | 297,282 | 281,934 | 261,461 | 268,219 | 270,498 |
| Fund Balances | 8,590 | 5,093 | 3,924 | 6,006 | 11,218 | 10,651 | 8,076 | 11,281 |
| Total Liabilities and Fund Balances | 266,914 | 270,622 | 283,440 | 303,288 | 293,152 | 272,112 | 276,295 | 284,964 |
| STATEMENT OF OPERATIONS | ||||||||
| For the year ended March 31, (Amounts in $ thousands) | ||||||||
| 2018 | 2017 | 2016 | 2015 | 2014 | 2013 | 2012 | 2011 | |
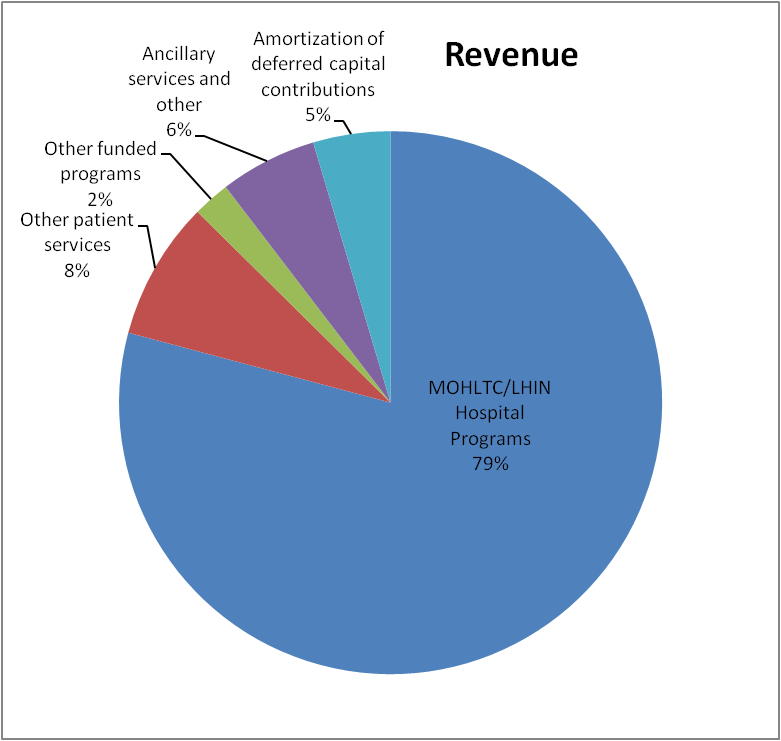
| Revenue | ||||||||
| Ontario Ministry of Health and Long-Term Care / North West Local Health Integration Network |
275,339 | 257,692 | 258,582 | 249,780 | 238,968 | 233,940 | 227,104 | 221,085 |
| Other patient services | 28,706 | 27,994 | 26,809 | 26,841 | 26,411 | 25,109 | 26,716 | 26,721 |
| Other funded programs | 7,689 | 7,693 | 11,593 | 10,863 | 9,671 | 8,838 | 8,727 | 7,312 |
| Ancillary services and other | 20,112 | 22,121 | 19,954 | 17,681 | 17,020 | 15,532 | 16,246 | 15,117 |
| Amortization of deferred capital contributions | 16,024 | 15,597 | 15,953 | 16,253 | 16,214 | 16,767 | 16,420 | 19,738 |
| 347,870 | 331,097 | 332,891 | 321,418 | 308,284 | 300,186 | 295,213 | 289,973 | |
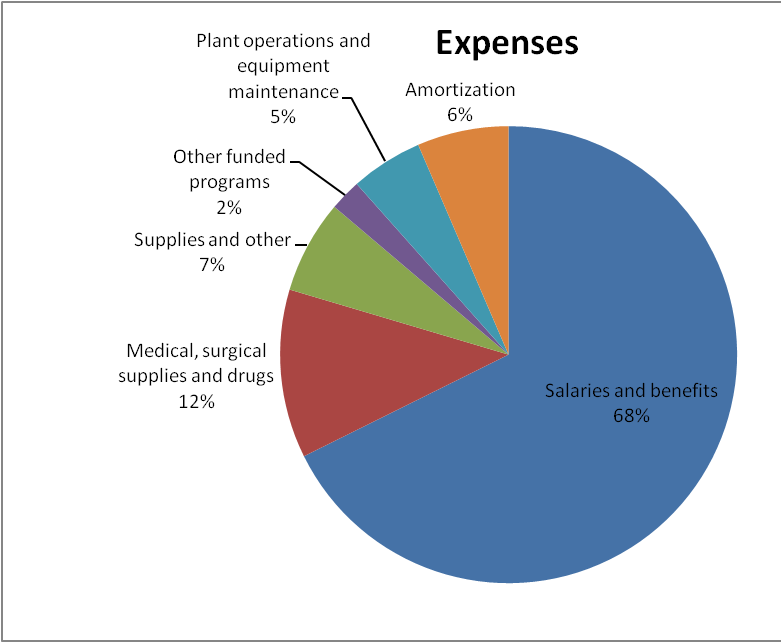
| Expenses | ||||||||
| Salaries and benefits | 233,900 | 223,589 | 221,916 | 213,384 | 204,366 | 198,443 | 200,141 | 195,068 |
| Medical, surgical supplies and drugs | 41,233 | 37,409 | 38,315 | 40,059 | 36,064 | 34,486 | 34,919 | 33,866 |
| Supplies and other | 22,834 | 23,386 | 22,653 | 19,416 | 19,216 | 18,089 | 22,666 | 21,665 |
| Other funded programs | 7,689 | 7,702 | 11,764 | 10,981 | 9,647 | 8,840 | 8,744 | 7,226 |
| Plant operations and equipment maintenance | 17,624 | 17,643 | 17,687 | 17,665 | 16,252 | 15,874 | 10,517 | 13,614 |
| Amortization | 22,384 | 21,818 | 21,284 | 22,086 | 22,758 | 22,032 | 21,245 | 20,868 |
| 345,664 | 331,547 | 333,619 | 323,591 | 308,303 | 297,764 | 298,232 | 292,307 | |
| Excess (deficiency) of revenue over expenses | 2,206 | (450) | (728) | (2,173) | (19) | 2,422 | (3,019) | (2,334) |