Thunder Bay Regional Health Research Institute
Our Mission
To be an international leader in health technology research and other strategic health innovation, that improves the health of the people of Northwestern Ontario and others.
Our Vision
Bringing Discovery to Life
Our Values
Excellence
Collaboration
Innovation
Integrity
Respect
Accountability
Our Philosophy
Patients and Families are at the centre of everything we do.
About us:
Incorporated as the Thunder Bay Regional Research Institute in December 2007 and renamed the Thunder Bay Regional Health Research Institute in November 2016, the program is the research arm of the Thunder Bay Regional Health Sciences Centre. Its mandate is to facilitate clinical research –particularly in the area of imaging and related fields – strategic to regional health care needs. Current research areas include but are not limited to cancer, cardiac disease, stroke, orthopaedics, Indigenous health, and lung disease. The Health Research Institute also supports clinical trials at the Health Sciences Centre, which has been in Canada’s Top 40 Research Hospitals since 2010 thanks in large part to the activities of the Health Research Institute.
The Health Research Institute aims to develop innovative health care techniques from concept to clinical trials to commercialization, supporting scientists and clinicians at every step. As of 2016, the Health Research Institute has spun off two companies, XLV Diagnostics and Radialis Medical, with others to follow.
Our Last Five Years in Review
With this Annual Report we close the final chapter of the Thunder Bay Regional Health Research Institute’s 2012-2016 Strategic Plan. The plan outlined three goals in our mission to create a patient-centric research program that would benefit the residents of Northwestern Ontario and create new and innovative diagnostic techniques to benefit the world. We are pleased to announce that we’ve been successful in that mission.
Our accomplishments include (to name just a few) the installation and commissioning of our new cyclotron, the formation of two spin-off companies (XLV Diagnostics Inc. and Radialis), our rise to 35th of the Top 40 Research Hospitals in Canada, and an ever-expanding roster of clinicians who are partnering with us to provide better care for our patients.
Creating a research institute is an extremely difficult proposition, especially when you are building something new that doesn’t fit the traditional mould. What we’ve accomplished so far is astounding. We have formed a successful research hub outside of a major metropolitan area, focused on innovative ways to collaborate and build capacity, and – most importantly – remained patient-centric. Of course, none of this would be possible without our numerous funding partners.
The next Strategic Plan will guide us over the next five years as we build upon these successes.
Leader Messages
Message from the Chair
Leading the Way in Patient-Centred Research

Looking back on my years as Board Chair, I’m both amazed and proud of the changes we’ve seen. We continue to focus our efforts on an area of research you don’t hear too much about in the Canadian Medical Association Journal or Scientific American: patient-centred research that addresses the immediate needs of the local and regional population.
This may sound too specialized to have a global impact, but the fact is that some of the new equipment and health care pathways being developed in Thunder Bay will have applications around the world. XLV Diagnostics Inc. and the relatively new Radialis Medical Inc. are two high-profile examples.
But there are other examples too, as you’ll read in this Annual Report. Our scientists are finding new ways of using High Intensity Focused Ultrasound as a safe and minimally invasive treatment option for many conditions and patients including newborns. Other research projects are helping us overcome barriers to Indigenous health in Northwestern Ontario, which will have applications across Canada and around the world. We are pushing the boundaries of distance health care thanks to our research into ways of providing effective health care to the 250,000 people who live in Northwestern Ontario – an area the size of France. We are also blazing the way for hospital-based cyclotrons, and our efforts installing our own cyclotron over the last several years have helped develop the blueprint for other hospitals in Canada to follow.
I am pleased to be joined this year by two new leaders who will take us through our 2020 Strategic Plan. Jean Bartkowiak became the new CEO for both the Institute and the Thunder Bay Regional Health Sciences Centre last year. He, too, is eager to align the priorities of both organizations as we continue to integrate more closely. Dr. Abraham (Rami) Rudnick will be another strong ally, bringing with him a wealth of knowledge and experience in both distance health care and Indigenous health.
As we enter this new era, we also end another. Today we say farewell to some of our Board Directors. Each has been part of this Board of Directors since its inception, and that is an exceptional commitment. To Keith Jobbitt, Michael Julius, Robert Paterson and Lou Siminovitch, thank you for building our Institute into the success we celebrate today. It has been an extraordinary nine years, and I hope that, as your terms conclude, you look back on all we have accomplished with a great sense of pride. Your role in developing this organization from the ground up cannot be understated, and will continue to have an impact well into our bright future. It is fitting, then, that we have contributed $500 in honour of each of you to the student bursary fund at the Northern Ontario School of Medicine. Thank you for all you have done.
I would like to also take this opportunity to thank the entire Board and everyone at the Institute and the Hospital for their support during my tenure. I know I leave the Board – and the Institute itself – in good hands.
Dr. Gary Polonski
Chair
Message from the CEO
A New Vision, A New Plan

From the start, the Thunder Bay Regional Health Research Institute focused on health challenges that affect us most in Northwestern Ontario. We have sharpened that focus through collaborations between our scientists, clinicians at the Thunder Bay Regional Health Sciences Centre and elsewhere, and by understanding the shared priorities of the Health Research Institute and the hospital. Today, we are developing new and innovative techniques for universal health care challenges such as cancer care. But just as importantly, we are also creating Thunder Bay solutions to our own unique challenges including barriers to Indigenous health and providing distance health care for patients across our large region.
To help us achieve this vision, I am pleased to welcome our new VP of Research and Chief Scientist, Dr. Abraham (Rami) Rudnick, who formally joined our team on January 3, 2017. His focus on Indigenous health, belief in aligning research and hospital priorities, and his ability to engage stakeholders at every level are exactly the qualities we need moving forward. Already his experience with Indigenous health and distance health are having a large impact on the way we conduct research and deliver health care.
Rami’s work has contributed to a meaningful and focused new 2020 Strategic Plan. Our nine goals fall under three pillars: Healthier, Wealthier, and Smarter. These goals align closely with the hospital’s own 2020 Strategic Plan and priorities: Indigenous Health, Seniors’ Health, Acute Mental Health, and Comprehensive Clinical Care. To reflect our ongoing integration with the hospital, we added the word “Health” to the Thunder Bay Regional Health Research Institute name in fall 2016.
Finally, I would like to recognize our esteemed colleague and Chair of the Health Research Institute Board, Dr. Gary Polonsky, who is stepping down this year. His guidance and insights over the last several years of change for our Institute have been invaluable. Gary leaves us well-positioned to successfully tackle our new Strategic Plan and to take the next step in our growth. Thank you, Gary, for helping us make patient-centred research the success it is today.

Jean Bartkowiak
CEO
A message from the Thunder Bay Regional Health Sciences Foundation
CLOSER-TO-HOME RESEARCH FOR CLOSER-TO-HOME CARE
Research drives better patient care. In turn, local research drives better local patient care. That’s why the Thunder Bay Regional Health Sciences Foundation invests so much in local research. By supporting the Thunder Bay Regional Health Research Institute, our donors help improve the level of healthcare in Northwestern Ontario right now and in the future through research breakthroughs, better equipment, and attracting the high-calibre healthcare professionals that make such a difference in our lives.
Recently the Health Sciences Foundation has partnered with the Board of Directors of the Thunder Bay Regional Health Research Institute to host events that have introduced the revolutionary research happening in Northwestern Ontario to an audience outside our geographical area. These events have sparked discussion about how we can tackle the specific health care issues facing our geographic area. Specifically, how can research improve the health of our Indigenous population? There is a tremendous opportunity to work together to reexamine how research partnerships can exist to transform care.
Our focus is always on closer-to-home patient care. Supporting local research is yet another way of realizing that vision.

Healthier
Enhance research to improve the health outcomes of the people of Northwestern Ontario and beyond.
Partner with Indigenous researchers and communities to advance their health priorities.
Investigate and apply assessment and intervention solutions that are responsive to our geographic challenges.
Strengthen local clinical research.
Dr. Naana Jumah Receives CIHR Grant to Create New Care Models during Pregnancy in Rural Northwestern Ontario
It’s a number that made national news: up to 30% of pregnancies in Northwestern Ontario are to mothers with opioid addiction.
“It is a shocking number, yes, but given the overall rates of opioid use in our region both within Indigenous communities and non-Indigenous communities, I don’t think we should be surprised that it is that high,” said Dr. Naana Jumah, an obstetrician at Thunder Bay Regional Health Sciences Centre and a clinician researcher at the Thunder Bay Regional Health Research Institute.
In 2016, Dr. Jumah received a research grant of almost $500,000 from the Canadian Institutes of Health Research (CIHR) to help mother and baby. Newborns of opioid-dependent mothers may suffer from withdrawal symptoms after birth. Part of the problem is that there isn’t a standard of care that takes into account all of the combined challenges.
“Right now we don’t have guidelines that address the needs of women in rural and remote communities who have substance use and mental health issues during pregnancy,” Dr. Jumah said. Her research to this point has included investigating substance use – particularly opioids – among pregnant women in rural areas to find out exactly what the challenges are.
The CHIR grant will take that research to the next level, funding a holistic, multi-pronged project to find ways of overcoming them. The goal is to create an evidence-based model of care that addresses the complex and connected challenges including distance barriers, cultural barriers, and other social determinants to health, as well as the medical issues surrounding substance use in pregnancy. Ultimately, this will improve patient care for mother and child.
One area of research is a grassroots project already launched by the Shibogama First Nations Council. This group of five fly-in First Nations was developing an integrated care pathway for pregnant women who have to travel to Thunder Bay due to the complications that arise from opioid use. Unfortunately, funding ran out before the project was completed.
“It’s a really good piece of work that they did, and it would benefit not just the women from their Tribal Council, but so many women from the North who have to travel to deliver,” Dr. Jumah said.
What makes this model of care unique is that the First Nations are developing it themselves. “We’re looking at health in a different way. It’s about caring for people and their well-being while being respectful of their culture and their traditional ways of knowing. I’m there to provide support.”
Another area of Dr. Jumah’s research is to find a way to help Indigenous women get care in their own communities rather than travel for every appointment.
“Right now expectant mothers have to fly out, sometimes for three or four days, every time they have an appointment. That’s very disruptive to their lives. We want to find ways to help women stay in their communities more during pregnancy,” Dr. Jumah said.
Telemedicine services may provide one of the answers. Dr. Jumah will explore a variety of possible uses for videoconferencing technology from prenatal appointments to group information sessions and mental health and addictions support.
Dr. Jumah said that ultimately, this research will help provide better care for all pregnant women living in remote communities and especially those with addiction issues. She is also hoping to change the way in which research is conducted so that it is more respectful of Indigenous values.
“The overall approach to this grant and to my research in general is to use a more Indigenous-based worldview to the research – respecting the foundational ideas that are inherent to many Indigenous communities.”

Dr. Naana Jumah received a research grant of almost $500,000 from the Canadian Institutes of Health Research (CIHR) to develop a standard of care in rural areas for opioid-dependent mothers during pregnancy to help mother and baby.
Exploring Respiratory Disease in Canada’s Indigenous Population: Health Research Institute Partners with Fort William First Nation
The prevalence of asthma and chronic obstructive pulmonary disease has increased amongst Indigenous populations. To figure out why and what to do about it, the Thunder Bay Regional Health Research Institute has partnered with Fort William First Nation.The prevalence of asthma and chronic obstructive pulmonary disease has increased amongst Indigenous populations. To figure out why and what to do about it, the Thunder Bay Regional Health Research Institute has partnered with Fort William First Nation.
“Indigenous populations have a unique set of health issues which we would like to help reconcile through this study,” said Dr. Mitch Albert, Ph.D, Director of MRI Research, Health Research Institute. “Our hope is to raise awareness about respiratory health amongst Indigenous communities, thus increasing the likelihood of them accessing care.”
Fort William First Nation will help recruit both healthy volunteers, and people who suffer from various lung disorders from their community to participate in the study with the Health Research Institute. The findings will then be compared against the findings of non-Indigenous volunteers. Chief Peter Collins of Fort William First Nation will work closely with the Health Research Institute to help develop the clinical protocols.
The aim is to determine an optimized set of MRI scan parameters that will produce clear, anatomically and clinically relevant images of the lungs for healthy participants and participants with various lung disorders. The results are expected to provide unprecedented information on the extent of respiratory disease progression in people of Indigenous descent.
“This study has the potential to improve the respiratory health status of our Indigenous patients and families,” said Dr. Albert. “We couldn’t do this important work without the support of Fort William First Nation and I’m so thrilled to partner with them on this endeavour.”

(From left to right) Chief Peter Collins of Fort William First Nation and Dr. Mitch Albert, Ph.D, Director of MRI Research, TBRHRI
Targeted treatments for cancer caused by human papillomavirus (HPV)
Our scientists are developing new, less invasive treatment options for patients with HPV-related cancer. Dr. Ingeborg Zehbe and her team are researching drugs which specifically target the virus to stop cancerous changes in the infected cells.Human papillomaviruses (HPVs) are some of the most common sexually transmitted viruses in the world. Chronic infections with certain types of HPV are responsible for causing almost all cases of cervical cancer as well as a growing number of head and neck cancers, which can affect both women and men.
Currently, abnormal changes in cervical cells, which indicate an HPV infection is present, are detected through routine Pap testing. Patients are then monitored to determine whether their immune system can eliminate the virus or cancer will fully develop. If cancer does develop, available treatment options include surgery, chemotherapy, and radiation – all of which are invasive and cause many unwanted side effects.
Scientists at the Thunder Bay Regional Health Research Institute are developing new, less invasive treatment options for patients with HPV-related cancer. Dr. Ingeborg Zehbe and her team are researching drugs which specifically target the virus to stop cancerous changes in the infected cells.
What makes this research especially exciting is the way the treatment is given – and it’s an excellent example of the collaborative nature of our Health Research Institute.
The Health Research Institute is a close working environment where scientists talk with each other, often leading to new innovations. In this case, Dr. Zehbe, a cancer biologist, has teamed up with scientists Dr. Laura Curiel and Dr. Samuel Pichardo, both of whom are engineers and experts in high-intensity focused ultrasound (HIFU). Together, they have created a unique way delivering the HPV-targeted drugs into cancer cells using a new HIFU technique. Unlike traditional chemotherapy and radiation treatments, this treatment will have minimal side affects on surrounding healthy tissues, greatly improving patient experience.
Dr. Zehbe and her team are working to perfect the therapy thanks to funding from a Collaborative Health Research Projects grant, a joint initiative between the Canadian Institutes of Health Research (CIHR) and the Natural Sciences and Engineering Research Council of Canada (NSERC). The goal is to make therapies such as this a part of everyday health care, improving patient experience and outcomes while also reducing health care costs. It’s another way we are Bringing Discovery to Life.

Thunder Bay Regional Health Research Institute – Lakehead University Research Chair Dr. Ingeborg Zehbe (left) and members of her team including PhD candidate Melissa Togtema (right) are making less-invasive treatment options possible for patients who develop cancer due to a chronic HPV infection. Their research focuses on the development of drugs that specifically target the virus to stop it from causing cancerous changes in infected cells.
Wealthier
Enhance philanthropic support and generate revenue through science and partnerships.
Engage stakeholders in philanthropy and other support of research.
Develop health technology products and assets.
Secure a robust clinical trials program.
Cyclotron Produces First FDG – but Program Development is the Real Story
The cyclotron passed a major milestone in 2016, delivering its first radioactive isotope (an atomic variant of an element) fluorine-18 for research and calibration purposes. Now, an application is pending with Health Canada to produce the radiopharmaceutical fluorodeoxyglucose or FDG for patient use. Stephen Exley, Interim Director of Cyclotron Operations, emphasized that the real achievement is the homegrown cyclotron program itself.
“The team has taken so much knowledge from other sources and brought it together to create this unique program,” Exley said. “The end product, FDG, is a relatively simple radiopharmaceutical that is extremely useful. But it’s the seven years of preparation including constructing the bunker and developing the program – that’s what people don’t always see. For this team to acquire all that knowledge and put it together is incredible.”
FDG is used to “light up” cancer cells during positron emission tomography (PET) imaging for cancer diagnosis, treatment planning, and treatment monitoring. Having a steady supply across the parking lot rather than across the province will reduce delays to patient care.
Thunder Bay Regional Health Sciences Centre is one of the first hospitals in Canada to build its own cyclotron program for patient care and research. It’s for that reason that there was no real blueprint for creating such a program. Terry Fodë, Project Support Officer, said that the public engagement piece of the Thunder Bay experience – which she spearheaded – will be used for current and future programs nationwide.
“The Canadian Nuclear Safety Commission (CNSC) deemed our public information program as a ‘gold standard’ and requested to use it as a template for the rest of the cyclotron facilities across Canada,” Fodë said.
What is perhaps most remarkable is the fact that most of the staff running this complex facility are from Thunder Bay. Given the technical expertise and knowledge needed, it is a testament to how far Thunder Bay has come, Exley said.
“You can see the growth and evolution of the people here to develop the program and facility,” he said.
One of those local people is Dr. Jesse Walker, a Cyclotron Associate and recent PhD graduate in Chemistry from Lakehead University. When he started his university career, there weren’t many opportunities in Thunder Bay in his field – he expected he would have to leave town. With the launch of the cyclotron program, Dr. Walker had the opportunity to stay at home.
“When I started in the PhD program, I knew it would be challenging to find a position in Thunder Bay,” Dr. Walker said. “I wanted to pursue a career that involved medicinal chemistry, so this really was a great fit for me.”
Cyclotron Associate Melissa Quance is also from Thunder Bay. Dr. Michael Campbell, who oversaw the cyclotron’s construction, is now the Lakehead University – Health Research Institute Research Chair in Radiochemistry and remains the program’s Radiation Safety Officer. In fact, only three staff members are not from the area: Fodë (though she has been in Thunder Bay for eight years), Sonja Desjardins, a Cyclotron Associate and the Deputy Radiation Safety Officer who is from Sudbury, and Bozin Nedanovski, the Cyclotron Equipment and Safety Systems Manager who is from Italy and came to Thunder Bay initially as part of the installation team. Most have science backgrounds including chemistry, physics, and biology, and each member of the team specializes in important areas of the cyclotron operation.
And that’s just the tip of the iceberg. As production increases, more technicians will be needed, and there’s every expectation that these specialized jobs will be filled by local residents as well.
“All the knowledge that goes into producing radioisotopes was learned by local people,” Exley said.

Stephen Exley (right), Interim Director of Cyclotron Operations, said that the real accomplishment is the homegrown program – one of the few hospital-based cyclotron programs in Canada. Dr. Jesse Walker (left) and Terry Fodë are part of the team that built the program essentially from the ground up.
Health Research Institute/Sunnybrook Collaboration Investigates New HIFU Treatment Option for Aggressive Cancer
Dr. Samuel Pichardo is helping oncologists at Sunnybrook Health Sciences Centre to explore new methods of using high-intensity focused ultrasound (HIFU) to help treat cancer tumours in patients.A new series of clinical trials now underway at Sunnybrook Health Sciences Centre has a strong Thunder Bay connection. Dr. Samuel Pichardo, a research scientist at the Thunder Bay Regional Health Research Institute, is helping oncologists at Sunnybrook Health Sciences Centre to explore new methods of using high-intensity focused ultrasound (HIFU) to help treat cancer tumours in patients.
Dr. Pichardo brings his HIFU expertise to the project, working with Dr. Justin Lee (head and neck cancers) and Dr. William Chu (rectal cancer) to develop a non-invasive clinical approach that would increase the effectiveness of chemotherapy and/or radiation therapy with minimal side effects.
“Thunder Bay is helping to write the new book for multimodal cancer treatments using HIFU,” said Dr. Pichardo.
The technique, which is called MRI-HIFU, combines magnetic resonance imaging (MRI) and HIFU to heat the tumour to about 43 degrees Celsius. This “sensitizes” the tumour, making the other cancer treatments more effective. In lab tests, this approach was shown to shrink the tumour size more than with radiation treatment alone.
These positive results prompted the Sunnybrook clinical trial. The study is aimed at patients who have a recurrent cancer that cannot be treated with surgery.
“These are the patients who have tumours that don’t respond as well or are not eligible for traditional treatments,” Dr. Pichardo said. “We are offering these patients another treatment method where the standard of care is not working as well as we would hope.”
As of mid-February 2017, three patients had been treated in the trial: two with rectal cancer and one with head and neck cancer. All three seemed to respond well to the treatment and had no side-effects due to the MRI-HIFU treatment – though it is too early to call the trial a success.
“The results for the two patients being treated for rectal cancer so far are promising; however we cannot come to any firm conclusions about the treatment’s effectiveness based on the results from so few patients,” he said.
If this new technique ultimately proves successful though, any hospital with MRI-HIFU capabilities and a radiation therapy treatment program – including the Thunder Bay Regional Health Sciences Centre – could adopt the new treatment method, helping prolong the lives of many cancer patients. Future clinical trials may include patients with less aggressive forms of tumours.

Dr. Sam Pichardo is helping oncologists at Sunnybrook Health Sciences Centre to develop a method of increasing the effectiveness of cancer treatments using HIFU.
Pre-Clinical Research in Thunder Bay into Combination Cancer Treatments Possibly a World First
A multi-institution research collaboration in Thunder Bay is looking at new ways of boosting cancer treatment effectiveness.Cancer cells have a natural defence against radiation therapy and chemotherapy – in fact all cells in the body have some sort of protection from harmful radiation and chemicals. One highly specialized research project happening in collaboration with several institutions in Thunder Bay may develop an innovative new way to break down those protections in cancer cells.
Or, perhaps more accurately, two new ways.
Dr. Simon Lees, a research scientist and associate professor at the Northern Ontario School of Medicine (NOSM), began by reviewing the literature that investigated the use of a sugar molecule called 2-DeoxyGlucose (2-DG) as part of a combination cancer therapy during radiation and chemotherapy treatment. This molecule essentially blocks cancer cells from using sugars, weakening their defences and in theory boosting the effects of cancer treatment.
Dr. Lees wondered if a similar approach could be researched in Thunder Bay.
“I knew from working with Dr. Chris Phenix at the Thunder Bay Regional Health Research Institute that we could make FDG in the lab (which is similar 2-DG) – we wouldn’t have to buy it,” Dr. Lees said. This “cold” FDG is the non-radioactive version of 18F, the radiochemical tracer used in PET imaging. “Other research has found that FDG might actually work better than 2-DG, and perhaps be less toxic.”
The pre-clinical research would investigate the effectiveness of combining FDG treatment with either chemotherapy or radiation therapy on human cancer cells (but not in the human body) with and without FDG. Dr. Lees partnered with Dr. Margaret Anthes, a radiation oncologist at Regional Cancer Care Northwest at Thunder Bay Regional Health Science Centre, for this phase of the project.
But Dr. Lees wanted to take the research one step further. As it happens, the Health Research Institute is also home to one of the world’s most advanced high-intensity focused ultrasound (HIFU) research programs. Dr. Laura Curiel and other researchers at the Institute are studying how HIFU can be used as a combination treatment with radiation therapy. HIFU warms the tumour cells to about 42 degrees Celsius, “sensitizing” the cancer cells in order to amplify the effects of radiation therapy. So why not study the results of combining all three?
“We are in a unique position to be able to do this type of research because we have all the equipment we need at the Research Institute (including HIFU, the microPET for monitoring tumour size, and the equipment needed to make FDG),” Dr. Curiel said.
Dr. Anthes, Dr. Lees, and Dr. Curiel received a Northern Ontario Academic Medicine Association (NOAMA) grant to conduct the study. As far as the researchers know, this will be the only research project in the world studying the effects of using all three treatments together.
“The first step we have to do is determine if the combination of FDG and radiation therapy is effective before we try all three,” Dr. Lees said. “We’ve already completed the early research where we verified that the FDG does inhibit glucose uptake in tumours for about two hours after injection.”
If successful, it could lead to Phase I clinical trials for cancer patients. The Clinical Research Services Department at the Thunder Bay Regional Health Sciences Centre has the capacity to participate in and even lead this type of clinical trial.
“We have the equipment and researchers who would be interested in pursuing it,” Dr. Lees said.
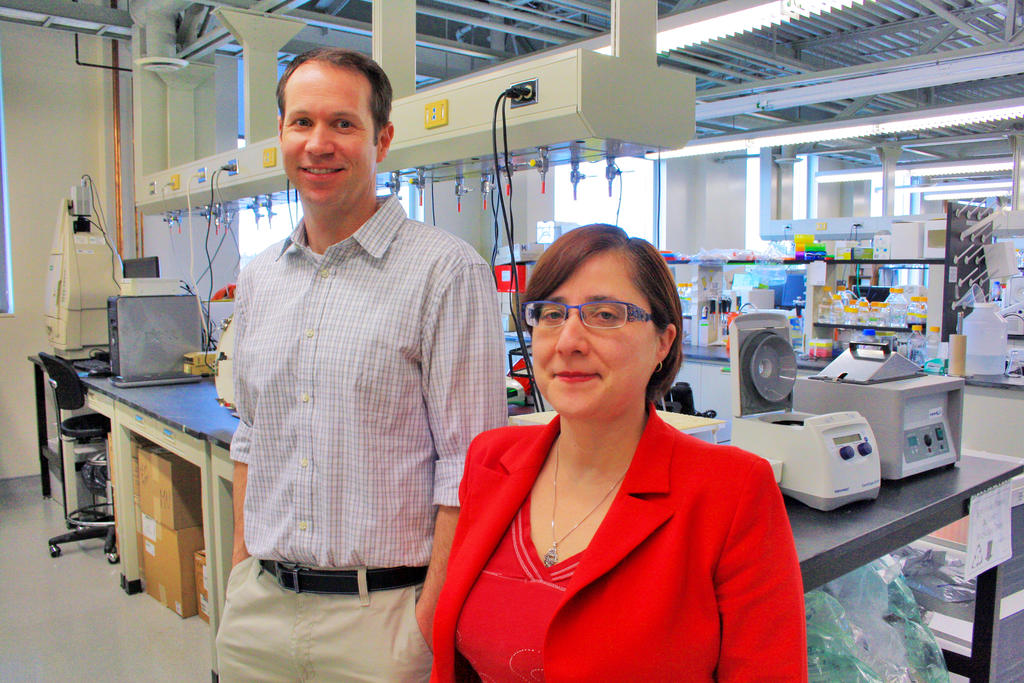
Dr. Simon Lees and Health Research Institute scientist Dr. Laura Curiel in the NOSM lab at Lakehead University. A multi-institution research collaboration in Thunder Bay is looking at new ways of boosting cancer treatment effectiveness.
Smarter
Enhance the academic environment.
Participate in development of academic programs relevant to our health research priorities.
Facilitate a research culture.
Grow strategic research partnerships and networks to expand research capacity and impact.
New Imaging Technique May Detect Alzheimer’s Disease Earlier
Is the future of early testing for Alzheimer’s disease being developed in Thunder Bay right now?
Dr. Mitchell Albert of the Thunder Bay Regional Health Research Institute and Lakehead University is heading up a team of researchers investigating a new method for detecting subtle changes in brain function. The method uses hyperpolarized (HP) xenon gas, a technique that Dr. Albert co-invented. When breathed in by the patient, the gas travels through the bloodstream and “lights up” areas of the brain during a functional MRI (fMRI) scan, providing up to 10 times more signal enhancement than traditional fMRI.
“For the first time ever, we were able to image the brain of an Alzheimer’s patient using HP xenon fMRI,” Dr. Albert said. As of February 2017, 18 individuals – a mix of healthy participants and those diagnosed with Alzheimer’s disease – had been scanned.
If the research is successful, HP xenon fMRI could be used for Alzheimer’s disease diagnosis and treatment monitoring. Although the research is far from complete, the results so far have been promising.
“What we found was that there were longer washout times (the amount of time it takes for the “lit up” area in an MRI image to fade) in participants with Alzheimer’s suggesting there is a slower blood flow in those individuals,” Dr. Albert said.
Signal enhancement is the key for early Alzheimer’s disease diagnosis using fMRI. It’s sort of like looking up at the stars. In Toronto, only the brightest stars can be seen so you don’t get a clear picture of the night sky. But in Thunder Bay, you can see whole constellations and even the Milky Way. In terms of fMRI, that means researchers – and eventually doctors – can see the brain function much more clearly, and be able to spot the telltale signs of Alzheimer’s disease in its earlier stages.
Early detection is important because although there is currently no cure for Alzheimer’s disease, there are treatments that are more effective the earlier the disease is diagnosed.
“This will perhaps allow us to detect the Alzheimer’s disease biomarkers that are crucial for identifying this disease at its early stage – much earlier than is currently possible,” Dr. Albert said.
The research would not be possible without a grant from the Weston Brain Institute, which provided $709,650 to fund the three-year project. The Institute commits more than $11 million each year to support innovative research into degenerative brain diseases.
“The Weston Brain Institute is pleased to support this kind of critical high-risk, high-reward work,” said Alexandra Stewart, Executive Director at the Weston Brain Institute. “If successful, Dr. Albert’s imaging tools will be of great impact in developing effective treatments for Alzheimer’s disease.”

Dr. Mitchell Albert received a Weston Brain Institute grant of $709,650 to study new ways of using HP xenon gas functional MRI for the diagnosis of Alzheimer’s disease and treatment monitoring. The research could lead to earlier detection of this devastating disease when it is more manageable.
PhD Candidate Researcher Pioneers “Agentless” Contrast Technique for Identifying Prostate Cancer
Chris Abraham, a PhD candidate working with Dr. Laura Curiel and Dr. Samuel Pichardo at the Thunder Bay Regional Health Research Institute, presented research in Vienna, Austria in 2016 that represents early steps to a whole new way of diagnosing and treating prostate cancer.Chris Abraham, a PhD candidate working with Dr. Laura Curiel and Dr. Samuel Pichardo at the Thunder Bay Regional Health Research Institute, presented research in Vienna, Austria in 2016 that represents early steps to a whole new way of diagnosing and treating prostate cancer.
Contrast in medical imaging is the ability to tell the difference between different kinds of tissues such as cancer cells and healthy cells. This helps doctors find cancerous tumours and plan treatments. In prostate cancer, magnetic resonance imaging (MRI) has difficulty showing the difference between malignant tissue and healthy tissue in the prostate because there isn’t enough contrast.
Abraham is investigating a new way to create better contrast by enhancing the “intrinsic characteristics” of each type of tissue to maximize contrast.
“There are many different variables that you can input into an MRI to change how the signal intensity looks,” Abraham said. A complex equation can be used to enhance minute differences between healthy and cancerous prostate cells to increase the contrast in the image. “We found that you can optimize the MRI parameters to create better contrast between the healthy prostate cells and cancer cells compared to conventional MR scans.”
It is groundbreaking research – Abraham said that he does not know of any similar research underway outside of the Health Research Institute. There is one significant drawback: the signal can be relatively weak compared to those using traditional contrast agents. However, the imaging technique offers several advantages. For one, contrast agents and biomarkers are difficult and expensive to develop. Further, some people can have bad reactions to contrast agents. This new approach solves both those problems since it can be used with any MRI unit without contrast agents. This technique could also be used with traditional contrast agents to enhance contrast even more.
Although the technique could be used as a diagnostic method, the real advantage could be to help target cancer cells during magnetic resonance-guided high-intensity focused ultrasound (MRgHIFU), which is an emerging treatment for some prostate cancer. Abraham is already researching possible techniques. The treatment might fully ablate (or “cook” at about 62 degrees Celsius) the cancer cells, or it might be used as a hyperthermia treatment (heating the cancer cells to about 43 degrees Celsius) to help improve the effectiveness of chemotherapy or radiation therapy. Hyperthermia has the potential to weaken the cancer cells and boost the body’s own immune system so that lower doses of radiation or chemotherapy would be needed, in turn reducing the associated side effects.
Both ablation and hyperthermia would offer the possibility of other treatment methods for prostate cancer patients to avoid nerve damage that is common in surgical treatments that can lead to sexual dysfunction, incontinence, and other issues.
“Survival isn’t enough. My motivation is to create a better treatment option using HIFU to avoid these complications.”
These uses are all still theoretical – clinical trials would be needed to develop any sort of treatment. Still, the research is promising. Abraham presented both research projects at the European Society for Magnetic Resonance in Medicine and Biology (ESMRMB) 2016 Congress in Vienna, Austria. Travel to the conference was provided through a grant from the Prostate Cancer Canada Network Thunder Bay.
Abraham is involved in five research projects at the Health Research Institute, all relating to HIFU, under the mentorship of Dr. Curiel and Dr. Pichardo. “They are amazing to work for. I wouldn’t be who I am without them.”
Other HIFU-related projects he is working on include biomarker research for prostate cancer and development of specialized MRI coils for HIFU treatment of paediatric neuroblastoma at SickKids in Toronto.
Chris Abraham, a PhD candidate at the Health Research Institute, presented his research on two topics related to prostate cancer at a conference in Vienna, Austria.
Researching How Technology Can Bring Health Care Closer to Home
Dr. Abraham (Rami) Rudnick wants to find even more ways of bringing health care to the patient through the use of technology.Travelling for health care is a given for many people living in Northwestern Ontario, though technology is helping reduce distance barriers to care. Dr. Abraham (Rami) Rudnick, who became the Vice President of Research for the Thunder Bay Regional Health Sciences Centre and the Chief Scientist of the Thunder Bay Regional Health Research Institute in January 2017, wants to find even more ways of bringing health care to the patient through the use of technology.
“Mobile and remote access can help improve health outcomes considerably. We want to do more, and do it in a more timely fashion: early detection, early intervention. Technology can help us do that as close to home as possible,” Rami said.
Northwestern Ontario tends to have poorer health outcomes than provincial averages for a number of reasons, and distance to health care services is a major factor. Although it’s not a unique problem (for example, Australia has a similar challenge), it is one that requires custom solutions. Today, videoconferenced family doctor and specialist appointments are becoming more common, and there are other tools to connect patients with doctors and other health care providers right from the patient’s home.
Rami wants to consider expanding the use of Internet-based tools including apps to help improve access to health care. “We can provide more care within remote communities,” he said. However, technology isn’t the whole solution. Instead, it is a tool to be used within a wider system of care. “We also have to look at how we can better use human resources.”
Although technology can improve access to care, there is a risk of imposing technology on patients, Rami said. That is particularly true when it comes to Indigenous Health. “The use of technology needs to be fully collaborative and based on the individual’s and community’s values, beliefs, and preferences.”
Education will be a key part of successfully integrating any use of technology, by care providers and learners as much as by patients.
“Research advancement is an opportunity to help health care providers to do research as well as to evaluate health care critically. That’s an example where partnerships with the Northern Ontario School of Medicine, Lakehead University, Confederation College, and others would work well.”
The goal would be to set up a collaborative remote health care system, easily accessible by patients and easily used by providers. Established alternatives such as satellite communication can be considered for communities that do not yet have access to broadband Internet.
“In the past, people talked about a hub-and-spoke model, but I don’t think that’s the right metaphor. I and others think about it more as a network. Some nodes may be larger in size, such as Thunder Bay, but there is fabulous research going on in some smaller nodes. Sioux Lookout, for example, has many health research projects.”
Rami has experience developing this type of remote health care model. As the Medical Director of Mental Health and Substance Use services at the Vancouver Island Health Authority, he helped guide the development of a freely available mental health promotion mobile app called BoosterBuddy, which supports youth and others who may be struggling with mental health challenges. He regularly involves patients and their communities in such research and development, which is part of the growing trend in health research in Canada and worldwide.
The BoosterBuddy app is just one example of how technology can help patients feel more connected. Technology can also help connect health care providers throughout the region, including researchers.
“It’s all about knowledge exchange and learning from each other.”

Dr. Abraham “Rami” Rudnick sees technology as one of the keys to overcoming Northwestern Ontario’s geographical barriers to health care delivery, and “improve health outcomes considerably.”
Strategic Indicators
Strategic Indicators are an essential element of strategic planning. Linked to Strategic Directions, Strategic Indicators measure performance, and provide a clear, meaningful gauge of performance over time.
In the 2016/17 fiscal year, a great deal of focus was placed on engagement with stakeholders to refine the Strategic Plan, and this resulted in the development of the following new Strategic Indicators. We look forward to reporting on progress in our 2017/18 annual report.
| Strategic Plan Alignment | Strategic Indicator |
|---|---|
| Healthier: Enhance research to improve the health outcomes of the people of NWO and beyond. | Percentage patient advised studies |
| Percentage Indigenous advised studies | |
| Percentage of patients participating in research | |
| Wealthier: Enhance philanthropic and other support and generate revenue through science partnerships. | Total number of participants enrolled in clinical trials |
| Total funding | |
| Clinical Research Gross Margin | |
| Smarter: Enhance the academic environment. | Total Trainees |
| # Faculty engaged in research | |
| # Peer reviewed joint publications |
2016-2017 Measures of Scientific Excellence
The following scorecard was applied to track progress in 2016/17
| Target | Actual | ||
|---|---|---|---|
| GOAL 1 - IMPACT THROUGH EXCELLENCE IN SCIENCE | |||
| 1.1 Focus on detectors, specialized MRI technology, molecular probes and imaging guidance. | |||
| 1.1A Research Grant Multiplier Research funding multiplier (cumulative this fiscal). The financial ratio measures the amount of times the scientists’ salaries are paid by the grant funding they have earned. This is operating funding, not capital. (cumulative as per MP) | x 1.5 | 1.05 | |
| 1.1B HQP Total number of TBRHRI Post Doctoral Fellows PDF’s working for a TBRHRI Scientist. Cumulative. (Total Trainees) | 1/number of Scientists (7) | 2 | |
| 1.1C HQP Total number of TBRHRI Graduate Students Master Students and PhD Students working for a TBRHRI scientist. Cumulative. (Total Trainees) | 2-3/number of Scientists (7) | 25 | |
| 1.1D HQP Total number of TBRHRI Undergrads/Volunteers Undergrands and volunteers, working for a TBRHRI scientist. Cumulative. | 3/number of Scientists | 51 | |
| 1.1E Number of publications in journals (includes any authors) Publication date must be in the time period being reported. Target of 3/per scientist/year. | 3/number of Scientists | 12 | |
| 1.2 Recruit and develop critical mass of internationally excellent scientists and trainees | |||
| 1.2A Implement 1 more TBRHRI-LU Research Chair TBRHRI-LU Research Chair contract in place. | 1 | 1 | |
| 1.3 Facilitate collaborations to increase success in scientific discovery, leading to first-in-patient trials and ultimately widespread distribution | |||
| 1.3A Industry Contribution to Science This includes revenue from commercialization activities, contract research, other industry science contributions to science accrued during period in question. This does not include clinical trials revenue nor does it include fundraising. | $100,000 | $13,372.00 | |
| GOAL 2 - ENABLING OF RESEARCH STRATEGIC TO TBRHSC | |||
| 2.1 Facilitate clinical research through an accessible, well managed, and sustainable infrastructure | |||
| 2.1A Number of participants accrued in clinical trials (Number of subjects enrolled in Clinical Trials) Number of participants accrued to any clinical trial. This includes TBRHSC as well as outpatient studies (i.e. TBRHSC privileged physicians are the principle investigator, but the patients are not necessarily active patients of TBRHSC. The count excludes patient accruals to clinical research studies not run through the Clinical Trials Department (e.g. patients enrolled in a study with Big Thunder Orthopedics). | 268 | 167 | |
| 2.1B Growth in patient accruals to clinical trials Report cumulative growth in patient accruals as of quarter in question, compared to previous fiscal.Patient accrual growth target 10 % as per TBRHSC briefing note and TBRHSC scorecard reporting. | 10% | 62% | |
| 2.2 Encourage emergence of research champions to grow culture of research | |||
| 2.2A NEW: Total number of Researchers who conducted research at TBRHRI and TBRHSC (Number of faculty engaged in Research) "A PhD or MD, who has over $500 in funding, is either a PI, QI, or SubI, cumulative throughout the year, (+TBRHRI Scientists)" | in Development | 90 | |
| 2.2B NEW: Total number of all Other Research Staff Any other person conducting research at TBRHSC, that is a SubI or PI with money. Included are CRA’s, CRC’s, CRS Physician Research Assistants, TBRHRI Research Associates/ Assistants that are directly related to the research. | in Development | 199 | |
| Total Research Staff (1.1B + 1.1C + 2.2A + 2.2B) | 301 | 316 | |
| 2.3 Enable clinical trials and clinical research in TBRHSC priority areas (Chronic Disease Prevention & Management, Comprehensive Clinical Services, Indigenous Health, and Mental Health & Addictions). | |||
| 2.3A Regulated Investigator initiated trials Active trials, e.g. HIFU for uterine fibroids and Skin Prep Solution Study (SPS), within the quarter. This count includes all active open and accruing Investigator Initiated Trials - Regulated only | 4 | 2 | |
| GOAL 3 - ECONOMIC GROWTH & SUSTAINABILITY | |||
| 3.1 Develop clinical trials, cyclotron, and other business ventures to reinvest in research | |||
| 3.1A Fully Implement Scientific Research and Experimental Development credits and leverage NW Medical Research Inc. SR&ED Net Revenue collected during period in question | "$180,000 " | $0 | |
| 3.1B Revenue from Clinical Trials / Clinical Research (Clinical Research Gross Margin) Gross Revenue from Clinical Trials/CR (including ICP revs etc) Earned during period in question. | $1,300,000 | $1,066,236 | |
| 3.1C Year-over-year growth of external research funding Research $ accrued in a quarter (i.e. not awarded). This would be funding from the private sector, external peer-reviewed granting bodies (including NOAMA), and peer-reviewed grants from charitable organizations (e.g. the Weston Brain Institute). Quarter to prior year quarter comparison. | 5% | 7.30% | |
| 3.2 Partner with TBRHS Foundation in research fundraising | |||
| 3.2A Amount of research revenue received from donors (Total Exernal Grants Contract & Funding) Report amount of operating revenue earned from donors during period in question ($300k from Foundation). This does not include funding for equipment. | $300,000 | $210,000 | |
| 3.3 Create value from intellectual property through spin-off companies and licenses | |||
| 3.3A Number of new patents issued (Number of Patents Awarded) Number of new patents awarded - by quarter (full / PCT patents only, not provisional | 1 | 0 | |
| 3.3B Number of provisional patents issued Number of provisional patents awarded by quarter | 2 | 2 | |
Financial Statements
Revenue Sources
Total = $6.7M
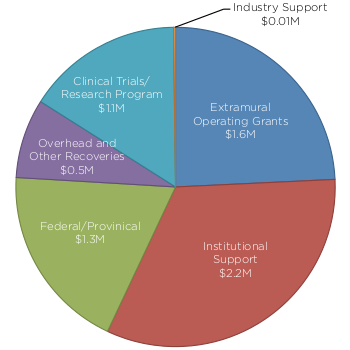
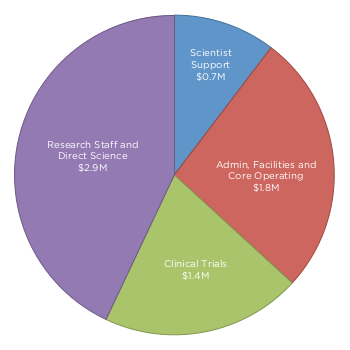
Expenses
Total = $6.7M